Improving Prescribing Error in a Paediatric Teaching Hospital
Improving prescribing errors in a paediatric teaching hospital, delivering targeted training for doctors and nurses to reinforce standards.
The Problem
Prescribing errors have multi factorial causes and have the potential to harm patients.
Prescribing is traditionally a relatively neglected skill amongst trainees. There is little in the way of formal assessment of prescribing practices. The RCPCH has formulated standards although these standards need to be implemented in the local context.
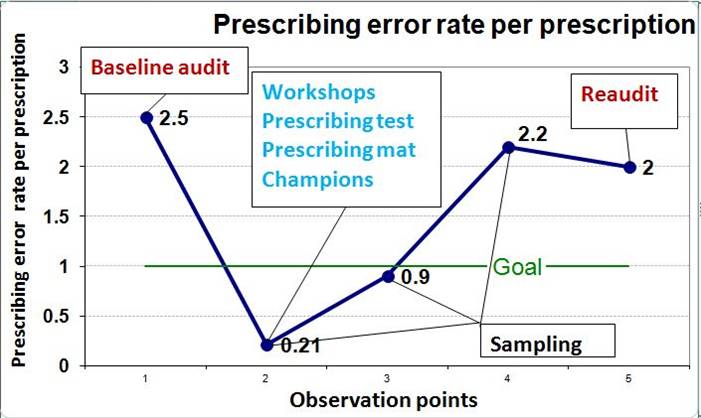
Local measurement with a baseline audit found a high average prescribing error rate of 2.5 discrete errors per prescription. The baseline audit demonstrated a need for supporting standards and training.
Aims
- To reduce prescribing error to below 1 per prescription by developing and implementing standards and delivering targeted training.
- To establish a multidisciplinary engagement in the department.
- To give regular feedback through sampling of prescription charts and re-audit.
Making the Case for Change
PDSA cycle 1 – Setting and teaching standards
- Prescribing standards based on national RCPCH and local guidelines were summarised on a ‘prescribing mat’ which was displayed in relevant clinical areas.
- Junior doctors performed a test based on the RCPCH prescribing guidelines and feedback was given.
PDSA cycle 2 – Developing the team and prescribing champions
- A multidisciplinary team of ‘Prescribing champions’ from volunteer doctors, nurses, pharmacists and managers was formed. A poster was designed with photos of ‘prescribing champions’ which also explained the project.
- Nurses received ‘microteaching’ during handover and were empowered to reinforce standards.
PDSA cycle 3 – Giving continuous feedback: sampling and re-audit
- Sampling of 5 prescription charts in weeks 2, 3 and 4 on all wards.
- Continuous feedback was given via ‘star chart game’ with ‘winner of the week’ poster award.
- Re-audit in week 6 of all drug charts.
- Qualitative survey of doctors/nurses.
Next steps: Establishing sustainability
Brainstorming with doctors/nurses to increase sustainability led to three action points:
- Implementing mandatory prescribing test at doctor’s induction.
- Providing all prescribers with stamps for signature legibility.
- Increasing ownership of stakeholders through- Junior doctors delivering teaching- Pharmacists taking on the role of sampling/feedback.
- Implementing zero-tolerance: If prescribing errors present then drug cannot be given until corrected.
Our Improvement
A significant improvement was demonstrated initially with a drop in error rate from 2.5 to 0.1 errors per drug. This result was not sustained over the next 6 weeks as the error rate gradually increased back to 2.0 as demonstrated in the re-audit.
Sampling of qualitative surveys (doctors and nurses) demonstrated that individuals increased their knowledge about prescribing standards and felt more empowered to implement them. The project supported multidisciplinary involvement and brought professionals together in the department.
Learning and Next Steps
What would we do differently next time?
- Smaller scale changes on one ward would possibly allow quicker changes followed by a phased ‘roll out’ to further wards.
- We measured process outcome but not outcome of less harm to patient which is difficult to measure.
We identify two key principles that made this project successful:
- Early involvement of a multidisciplinary team ‘prescribing champions,’ allowed collaboration between different professionals to endorse standards at different levels.
- Continuous feedback through sampling and the ‘star chart game’ was successful in keeping stakeholders informed and interested during the process.
The project has been approved by the paediatric department.
I would like to thank my supervising consultant Dr. Lucinda Etheridge for her support and advice, Dr Charlotte Verrill (FY1) and Dr Emily MacGregor (FY1) for collecting data (re-audit), Dr. John Wickenden and Dr. Nida Pasha for teaching and performing the prescribing test at induction, Mr Buddhi Pant (Assistant General Manager – Children’s Services) for support and practical help, Mz Efe Bolton (Principal pharmacist Women and Children Services) for advice and support and all ‘Prescribing Champions’ for their input and help.
Project lead: Dr Marianne Leach
Organisation: St George’s University Hospital Foundation Trust
