Module 2 – An Introduction to Improvement Science
Led by Nikki Davey, a Quality Improvement Practitioner and Coach, this second module in the QI series explores the science that underpins improvement, the challenges of starting small, and delves deeper into diagnostics and improvement methodology.
Introduction
At QIClearn we support paediatricians as they take their first steps in quality improvement, and even more. In the past 4 years we have seen over a hundred complete their first QI journey from start to finish. Most of these have recorded their journey in a poster and many have shared their work at international conferences.
Learning how to improve using a robust change method is a skill we can take with us throughout our career. In Module 1 in this series we looked at the way improvement science is one part of the tool kit that we use to deliver quality care to our patients. We looked at how the process of improvement mirrors the clinical journey, and we heard from paediatricians at different places on their own improvement journey.
In this module we will:
- Consider why we might need a robust change method and what we might gain from using one
- Explore the science that underpins improvement and look at one well-established improvement method
- Think about the challenge of starting small and how we can bring QI within our reach alongside our busy and demanding schedules
- Consider the best place to start our improvement journey and why diagnosis is as powerful a tool in QI as it is in clinical practice
- Dig deeper into diagnostics
- Have a go at ONE diagnostic tool
- Think about how we can make QI a habit that will stay with us throughout our career
This module is led by Nikki Davey, a Quality Improvement Practitioner and Coach. Nikki has a long association of working with paediatricians through her work in patient safety over many years. She founded the Quality Improvement Clinic in 2013 and has designed and delivered training to thousands of people since then. Through QIClearn, her company offers digital, virtual and blended programmes. Nikki is also a Trustee and longstanding supporter of the Clinical Human Factors Group who campaign for the adoption of human factors principles to make healthcare a safer place.
A robust change method
If we get on a roller coaster, we know that we will go up and we will go down, and that’s fun!
But when it comes to healthcare improvement and the health of others, we all want as smooth a journey as possible toward our goal. We can assess our progress by measuring what is happening. In order to intervene if things are going in the wrong direction, we will need to understand the normal variation in the process so we can tell if it is really changing.
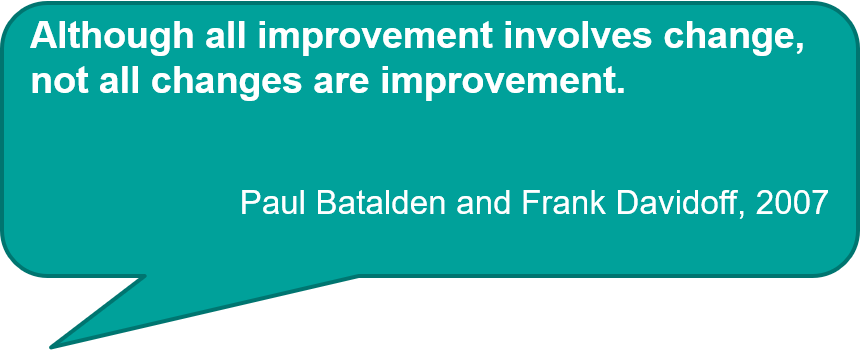
Robust change methods that draw on scientific principles such as the Model for Improvement include measurement in order to inform learning.
The Plan-Do-Study-Act cycle is part of the Model for Improvement. It’s the piece of the model that most people have come across. It has some similarities with other things we might be familiar with, such as audit, but it’s not the same.
Understanding how the Model for Improvement has come about can be useful, so the diagrams below provide some history in pictures from the early days of AUDIT promoted by Florence Nightingale to the divergence between LEAN methods and the Model for Improvement as they are applied in healthcare today.


3 questions, one learning cycle
In the video clip below, Nikki Davey describes the Model for Improvement, a scientifically informed change method that was developed by people who wanted to apply scientific principles to the process of change. As you might expect from a scientific method this involves measurement but, importantly, not the type of measurement that we are generally familiar with in healthcare!
The Model for Improvement was created by Langley, Nolan, Nolan, Norman & Provost and published in 1996. They added 3 questions to the learning cycle we know as Plan-Do-Study-Act or PDSA.
Nikki Davey introduces you to the model and provides a simple example to demonstrate how it works:
If you’re interested in hearing another person describe the Model for Improvement watch Dr Graham Mackenzie’s ‘An Introduction to Quality Improvement in 4 Every Day Objects’ video (13mins):
Start small
At QIClearn we invite people to Choose ONE thing, explore it more and then describe it in just 30 words before they embark on some diagnostics.
‘Small’ is a bit of a theme for us at QIClearn. Keeping things small at every stage is a way of conserving energy and not wasting any resources doing things we don’t yet know we don’t need to do!
Keeping things ‘small’ also helps us fail safe and learn fast – this is important as we don’t want the changes we make with the best of intentions to leave things worse than when we started. This is even more important if you are changing where you work frequently as you may never know the inconvenience or even the ‘little harms’ you left behind.
Here’s some advice from Dr Richa Ajitsaria, a Consultant Paediatric who mentors trainees as they have their first experiences of quality improvement:
How to ‘start small’
When we decide to embark on quality improvement we often have ambitions to make a BIG difference.
We have BIG IDEAS, and, if we allow it, our hearts rule our minds and we can get carried away….
One way to counter this natural tendency is by introducing some measurement. Measurement can bring objectivity into our choice about what to work on for our first QI project.
‘Choose ONE thing®’ is an activity that uses simple measurement to move from subjective to a more objective decision about what to work on. By scoring to three different dimensions and multiplying the scores you can generate a score that will provide a balance between where your heart and your head is leading you.
The three dimensions relate to the benefits for patients, our actual ability to fix things (as opposed to our imagined ability), and our motivation to take action.
Honesty is key here. It’s easy to over estimate our own sphere of influence to change things. And whilst we might be able to achieve change when we are on-call and working alongside the team, once we take a holiday or go to another team, the gains often disappear faster than they arrived. Good improvements on the other hand live on after we have moved on to our next team or next job.
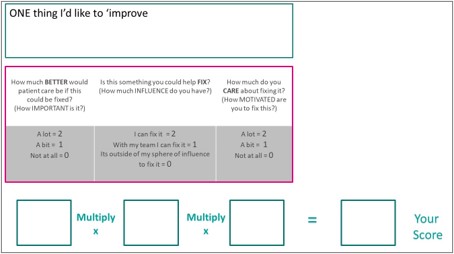
Here’s an example from Dr Georgina Ndukwe, a paediatric trainee we featured in Module 1:
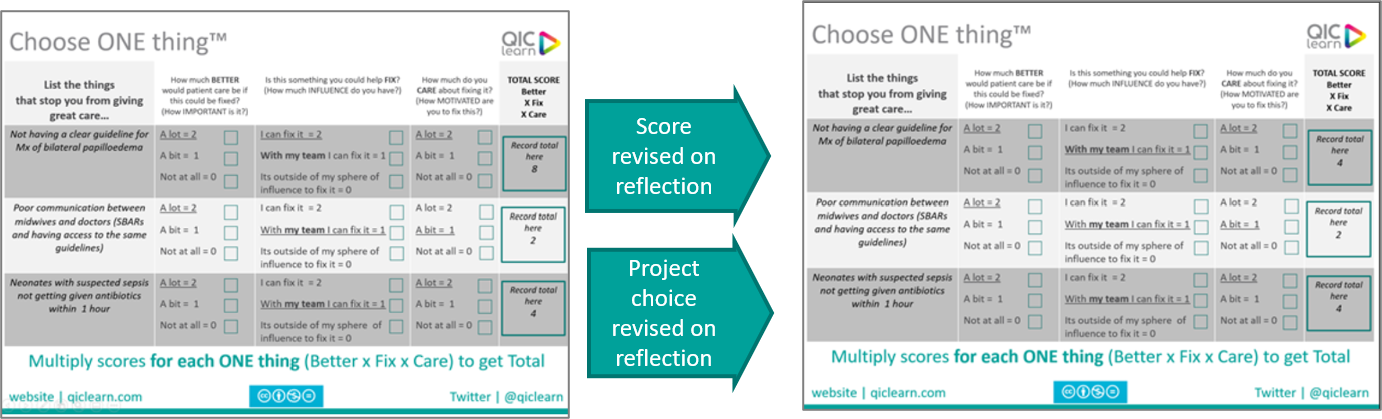
If you want to know more about how you can use it to get started with your QI project and see another version that takes audit recommendations as the starting point, you can sign up to QIClearn’s Getting Started with QI® and get free access to the tool.
The diagnostics
Stop before you start!
The authors of the Model for Improvement had a deep understanding of the diagnostics required to embark on any improvement journey and this is articulated in their book ‘The Improvement Guide’ (Langley, Nolan, Nolan, Norman & Provost, Josse Bass, 1996).
However, for those new to quality improvement, it is common place to dive straight into the aim without spending enough time on the diagnostics. In Module 1, we considered how diagnostics were as important in the QI journey as they are in the clinical journey.
We believe that adding a new question as a prequel to the Model for Improvement can be helpful. And so we ask: ‘What’s the problem?’ You can think of it as the diagnostics that you typically undertake when you first see a patient.

Digging into diagnostics
As with a clinical journey, diagnostics help us learn more about the problem we are facing. This in turn increases our chances of being able to achieve our goal.
The information you gain at this stage will help you engage others, and whilst you can learn the technical elements of quality improvement, in the same way that you can learn clinical skills, at the end of the day, a failure to engage the hearts and minds of others will often limit the benefits.
Whilst some improvement challenges might focus on meeting our own goals, we will achieve even more by purposefully choosing paths that deliver improvements for our patients too. Seeing the connection between the challenges we grapple with every day and the care we deliver can be helpful in bringing other people on board to help us overcome challenges.
The following 3 diagnostic tools all give us essential information that we should have before we go any further. As with clinical diagnosis, we may learn that the problem is not what we thought after all and have to change direction.
As you have already heard, improvement science is a learning activity. The method allows us to change our focus as more information emerges and we learn more.

Key features:
- Includes a START and END point
- Reads from left to right and sometimes contains spurs to other pathways and loop backs
- Maps the current process (work as is, not work as imagined)
- Can be annotated to indicate the focus of your improvement
- Shows steps before and after the focus point of improvement
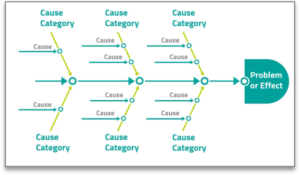
Key features:
- The problem is described in the fish head
- Causes are specific and written in terms of ‘deficit’ e.g. insufficient staff, time consuming to find a working computer, poor understanding of test schedule
- Causes are grouped together under common headings (categories are not fixed in stone)
- Causes are written on the spines under the category that fits best

Key features:
- Use small samples and collect data retrospectively
- Measure things like frequency or size of problem
- Use to differentiate between different segments e.g. patients with different conditions, different ages, different times of day
- Present bars in order from most frequent to least frequent
- Use a different colour to help your audience focus on the segment that interests you
Do ONE diagnostic thing
Whilst we recommend starting with the process map, all three diagnostics above are useful.
The fishbone diagram is often the diagnostic that people are most familiar with.
If you know about this and haven’t yet done one for yourself, or would like a refresher, check out this ‘3minuteQ’I video on how to do a fishbone diagram below:
Top tips for developing improvement habits
- Set an ambition within your reach – think microscopic
- Choose something you care about – keep motivated
- Grow your skills step by step – don’t overstretch
- Ask patients about their experience – from the start
- Use a robust change method – measure little and often
- Use simple language – avoid abbreviations
- Seek out people who are on the journey – shared wisdom saves time
Further reading
Fail safe, learn fast – Our motto for a great route to improvement


Module 2 reflection
Next steps
QIClearn courses
Module 3 - Involving Children and Young People in Your QI Journey
In collaboration with our children and young people's engagement team RCPCH &Us, the third of our QI online modules introduces healthcare professionals to involving children and young people in quality improvement and shares examples of different types of effective engagement.
Go to Module 3