Medicines Optimisation in Specialist Schools
A relatively new area for medicines optimisation where pharmacy workforce transformation can make a huge impact to support, tackle and raise awareness of health inequalities in the special education needs or disabilities sector, with a particular focus on improving medication safety standards and processes at school.
The Problem
Special schools are those that provide an education for children and young people (CYP) with a special educational need or disability (SEND). On 1st September 2014, Section 100 of the Children and Families Act 2014 placed a duty on governing bodies of maintained schools, proprietors of academies and management committees of pupil referral units (PRUs) to have in place arrangements to support pupils with medical conditions at their school.
Reducing health inequalities and improving health and wellbeing are major priorities for pharmacy. Pharmacists’ and pharmacy technicians’ skills of listening, explaining, advising and questioning are all highly relevant to help identify and support the medicines optimisation needs of CYP with complex health needs in special schools.
Within the collaborative commissioning structure between the NHS and Local Authorities for special schools, there has never been a formal pathway to promote or support the need for a pharmacy led medicines optimisation service in special schools. Hence, huge variations exist nationally on how this model is being delivered. Community health services play a key role in the future of health and care systems.
Aims
The primary aim of this project is to promote:
- Increased patient safety in schools through the development of a bespoke medicines optimisation service that allows for the improvements to upskill the unregistered teaching workforce in medicines administration, and a reduction in errors – e.g. omitted doses through medicines reconciliation provision
- Standardisation, consistency and equality of health provision across more special schools in Kent through recruitment of an additional Pharmacy Technician to complement the new service
- Development and transformational leadership opportunities for Pharmacy Technicians expanding on their traditional roles through working in a relatively untapped sector i.e. special schools promoting medicines optimisation.
Stakeholders
Stakeholders include:
- Local Authorities
- Schools – Headteachers and teaching staff
- Children and young people and their families including parents/carers
- NHS Commissioners and NHS Providers
- Community Pharmacies
The clinical intervention results achieved through this medicines optimisation project so far have all contributed as part of the building blocks to ensuring that the service supports CYP in special schools to have access to the; “right medication at the right time for the right reason.”
Feedback from one of our schools:
“Having access to the NHS Special School Pharmacy Service is the bonus service we did not know we needed; it has really added value and improved our practice. Since working with this service, we have improved our protocols around medication administration, our knowledge of medications, we have reduced the amount and type of medications given in school. The service is practical and helpful especially around medication queries & epilepsy / asthma plans. The technicians and pharmacists are always available and can be relied upon to get back to us to deal with enquiries and problems promptly.” – Milestone Academy Therapy and Health Team Lead.
PDSA Cycles / Solutions Tested
A quality improvement methodology and approach was undertaken for this workforce transformation project using the following tools:
- Driver diagram to produce a strategy for implementation of the new service over a phased period of time during the academic year (a copy is available in the full HEE report in the download section below).
- PDSA cycles to complete pre and post evaluation of medicines management practices as part of ongoing quality assurance monitoring.
- Logic Models to supporting clarity in thinking which enabled the development of appropriate evaluation strategies throughout the project.
Watch a short video created by the team about the project below:
Outcome Data
Medicines management quality assurance monitoring involved a baseline pre-audit of the sites at the outset, then followed up with a post project commencement audit to assess their compliance with the recommended guidance. The pre and post audit results below provides a graphic representation showing level of improvement following appropriate specialist pharmacy service support in areas including medicines management training, expert pharmaceutical advice, medicines related clinical interventions, guidance and support in policy and Standard Operating Procedure (SOP) development to improve standards across the schools:
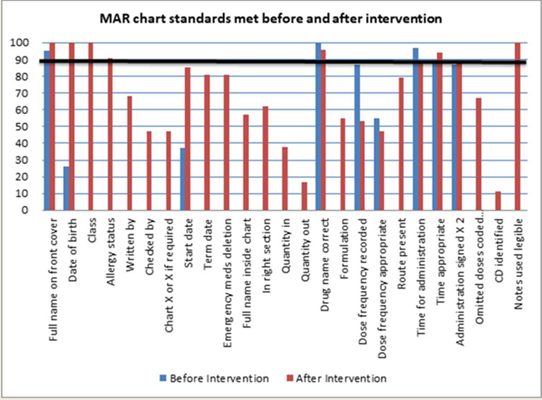
Four of the schools have demonstrated meeting above the 90% threshold for medicines management standards and two schools achieved 87% post implementation in comparison to pre-project review that identified a number of the schools were significantly below this threshold.
Following the baseline audits, the primary focus at the outset was to develop an overarching medicines policy through co-production with headteachers from all schools and the nursing teams. This was then followed by the development of bespoke SOPs for each school alongside the delivery of training in a blended format which included face-to-face, virtual and eLearning sessions.
Foreland Fields School was the pilot for eLearning with 100% of staff accessing this platform. Sessions were delivered by either pharmacy or nursing teams during COVID-19 pandemic restrictions when the pharmacy team were also responsible for supporting the COVID-19 Vaccination Programme. A total of 1,182 staff were trained across all 10 schools through the various training formats with the virtual sessions being most accessed (948 staff) due to the COVID-19 pandemic restrictions and approximately 60% of the training being delivered by the pharmacy team.
Clinical interventions undertaken by the team across all the schools over a 6-month period:
- A total of 232 interventions were made.
- Key areas where significant interventions were highlighted include emergency medication plan reviews for asthma (35%), epilepsy (32%) and specialist medical emergencies (23%).
Challenges and Learning
Challenges faced included unforeseen delays to the start of the project due to supporting the mobilisation of the COVID-19 Vaccination Programme. However, the team demonstrated excellent resilience during this time and developed a plan to ensure that once we returned to our business as usual there were steps in place to ensure the project timelines were on track.
The team also seamlessly integrated the COVID Vaccination Programme into the Special Schools work and supported the team with arranging the vaccination clinics including the preparation of vaccines as well as supporting school staff to work with the vaccinators in a way that best suited the children, young people and school environment with minimal distress and disruption. Uptake for majority of the schools for the COVID and Flu vaccinations were close to the local Kent and Medway average uptake (56%) and higher in some schools.
Medicines optimisation is about helping people to get the best outcomes from their medicines. It describes systems and processes used by staff, working in health and social care, which ensure that people receive the best possible care with medicines. The adverse effects of medications have been highlighted as a medication-related issue that can be a cause of both non-adherence and poorer school performance by CYP and parents/carers.
There is growing evidence base that further reinforces the need and importance of medicines optimisation in Special Schools through structured commissioning and collaboration with community pharmacies to provide:
- Repeat prescription service
- Effective medication reviews which includes considerations for deprescribing
- MAR Chart provision
- Medicines information and counselling
- Provision of suitable emergency medicine kits for salbutamol and adrenaline auto-injectors in schools.
These small but significant steps will support schools not only to effectively manage medicines that are essential during school hours but also support CYP to get the best outcomes from their medicines thereby promoting medicines safety in schools.
How This Improvement Will Be Sustained
Our next steps include continuing to build on this work locally and also support other special schools/pharmacy teams nationally through collaboration and sharing innovative practice as well as lessons learned. Closer integrated working with pupils, parents and carer involvement in focus groups are planned for the next academic year.
To support this work on a national and strategic level, the project lead has presented to MPs in the Westminster Forum in September 2021 when the SEND Policy Review was being discussed. Following this, invitations to speak at several schools and forums across the UK are planned throughout 2022 with the first one taking place in Greater Manchester.
A FutureNHS Workspace was recently set up for medicines optimisation in special schools to enable the collaboration to reach a wider audience through active engagement/networking, which will include working with national organisations such as the National Association for Special Education Needs (NASEN).
Closer integrated working with pupils, parents/carers involvement and co-production through focus groups are also planned for the next academic year.
Suggestions for Further Implementation
Tackling health inequalities is one of the key outcomes for the new NHS landscape that we are all embarking in to with the development and implementation of Integrated Care Systems (ICS). To support this agenda further, the team also plans to undertake more structured medication reviews with a primary focus on the STOMP-STAMP programmes.
STOMP-STAMP are about everyone working together to make sure children and young people get the right medication at the right time for the right reason. Overprescribing is not a new problem and a lot of great work has been done to address the issue. Healthcare professionals and NHS managers have been developing strategies for many years, and together with scientists, policymakers and patient representative groups have contributed to building up our understanding not only of the problem, and its consequences, but also of ways to tackle it.
The pharmacy team intend to implement Phase 2 of the project with a CYP and families centred approach through increased collaboration and co-production with key stakeholders to continue to ensure the safety of medicines in school as well as raise awareness and sharing learning on a strategic and national scale.
Presentation at Conferences or Meetings and Publications
- Poster presentation at Clinical Pharmacy Congress (13th-14th May 2022)
- Shortlisted for Clinical Pharmacy Congress Awards
- Entry submission to the European Society of Clinical Pharmacy 2022 Autumn Symposium (Prague)
- Speaker at Westminster Education Forum SEND Policy Reform Review Conference (September 2021)
- Opinion Article published in Royal Pharmaceutical Society Pharmaceutical Journal in February 2021: https://pharmaceutical-journal.com/article/opinion/children-in-special-needs-schools-urgently-need-more-pharmacist-support-to-take-their-medicines-safely
- Health Education England Pharmacy Workforce Transformation Initiative successful project bid for funding: https://www.lasepharmacy.hee.nhs.uk/workforce-and-quality/transformation/medicines-optimisation-in-special-schools/
- FutureNHS Collaboration Workspace: https://future.nhs.uk/connect.ti/MedOptimisationSpecialSchools/grouphome
Author: Nirusha Govender, Lead Pharmacist, Children, Young People and Dental Services
Organisation: Kent Community Health NHS Foundation Trust
Published: May 2022
