More than meets the eye: understanding the impact of guideline changes on retinopathy of prematurity screening performance
This QI project analysed National Neonatal Audit Programme (NNAP) ROP data to drive improvement and reduce the risk of preventable sight loss.
Publication date: 12 October 2023
Authors
Dr Julie Martin, Neonatal Clinical Fellow, Prof Rachel Pilling, Consultant Ophthalmologist, Neonatal Unit, Bradford Teaching Hospitals NHS Foundation Trust
Background
From 2018 to 2021,or the four years prior to 2022, National Neonatal Audit Programme (NNAP) data has shown that retinopathy of prematurity (ROP) screening for eligible babies has remained consistently between 95.1% and 95.7%. However, in 2022 the national average for on-time screening for ROP dropped to 69% and, in Bradford, we were screening 59.5% of babies on time.
There are two plausible explanations for this drop in performance:
- New national guideline1 recommendations (changing the eligibility threshold for screening from <32 weeks to <31 weeks), and
- narrowing the screening window from 3 weeks to a stringent window of 1 week, regardless of birthweight or gestation.
To drive improvement and reduce the risk of preventable sight loss, we interrogated our NNAP data.
Our improvement plan
We looked at each individual at-risk baby who was screened outside the window, to identify common themes that would be amenable to an intervention. We compared the NNAP data from the first half of 2022 to the second half of 2022, to evaluate the effect of implemented changes.
We identified that only three out of fifteen babies who fell outside the screening window were directly due to the change in screening criteria. The remaining babies did not meet audit standards either. This was because of incorrect BadgerNet documentation or having the incorrect date of the initial ROP screening booked in our ophthalmology diary. In Bradford, we use a spreadsheet-based individualised neonatal milestones calculator for all our babies, which includes the ROP screening window. Our improvement plan was two-fold:
- To update our milestone calculator to identify the correct screening window more clearly for each baby, and to amend the wording to reflect the specific Tuesday (ROP screening day in Bradford). The first ROP screen should be requested, rather than allowing team members to estimate.
- To provide unit education regarding documenting ROP screens in BadgerNet contemporaneously, while also designing a failsafe standard operating procedure for our ward clerks to check that this has been completed at weekly intervals.
Outcomes
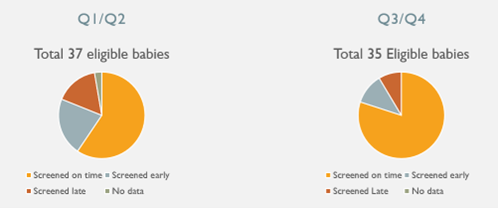
By making the changes above, we have shown a significant improvement. Bradford figures for on- time ROP screening have risen from 59.5% (below national average) to 80% (well above national average) between Q1/Q2 and Q3/Q4 in 2022 alone. There are no longer any babies without a documented first ROP screen.
To maintain our improvement, we have amended our ophthalmology diary to include the requestor’s details, to facilitate targeted feedback. We plan to continue to use our updated milestones sheet and ward clerk failsafe for BadgerNet documentation.
We are also working toward implementing a digital ROP screening pathway for our lower risk babies requiring ROP screening. A recurring issue is the provision of screening for infants who have been discharged prior to their screening window, which requires parents to attend the unit for assessment, often only days after returning home. We have a NeoForus camera within the department and are currently at the stage of training non-ophthalmology-based practitioners to take high quality retinal images for remote ophthalmology review. This will enable the Neonatal Department to support the Ophthalmology Service in delivering timely screening prior to discharge where appropriate, offering a degree of flexibility for parents and carers, so that ROP screening is not limited to one morning a week.
Furthermore, we provide teaching and local skills to our neighbouring special care unit at a time when the paediatric ophthalmology consultant outreach resource is diminishing, threatening the sustainability of neonatal (and therefore maternity) services. We hope that soon this will enable the most efficient use of staff resources and improve experience for parents, whilst maintaining best practice.
Challenges and learnings
By looking through each dataset, we found that there was more to the story and our initial hypotheses were only partly responsible for the drop in performance. There were simple ways to implement change and have seen an excellent improvement. We would like to see this improve again further into 2023 as we maintain the changes and begin to introduce the new digital ROP screening pathway. The changes were made possible by working closely with our ophthalmology colleagues to identify required changes and audit their impact.
Top tips for implementation
- Use the Royal College of Paediatrics and Child Health screening calculator2, or a local calculator, to determine an eligible baby’s first screening.
- Meet with your ophthalmology lead to discuss how you might work together to identify your individual unit’s challenges to achieving the ROP screening window.
- Use your NNAP data to support the identification of barriers to improvement.
References
RCPCH. UK screening of retinopathy of prematurity guideline. March 2022. Available at: https://www.rcpch.ac.uk/sites/default/files/2022-12/FC61116_Retinopathy_Guidelines_14.12.22.pdf
RCPCH. NNAP ROP screening calculator (MS Excel). Available at: https://www.rcpch.ac.uk/work-we-do/clinical-audits/nnap/measures
