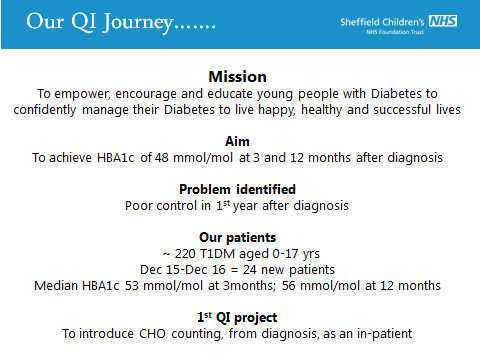
National Diabetes Quality Improvement Pilot: Our QI Journey So Far
Improvements in the first year of our QI journey following our participation in the pilot National Diabetes QI Collaborative in 2017.
The Initial Problem and its Impact
Our Diabetes Team look after approximately 220 Type 1 Diabetes patients aged 0-17 yrs. In the 2014-15 National Paediatric Diabetes Audit (NPDA) we ranked amongst the top 5 paediatric units with mean HBA1c <65mmol/mol. Subsequently our ranking slipped with increased mean HBA1c and fewer patients achieving HBA1c <58mmol/mol.
The invitation to participate in the pilot RCPCH National Diabetes Quality Improvement Collaborative offered us the opportunity to address our relatively poor outcomes.
Causes of the Problem
We recognised a particular problem with poor control in the first year after diagnosis and identified the need to drive change to be able to achieve improvement in outcomes for our patients.
We also identified the need to provide the patients with bespoke education that will empower them to manage their diabetes effectively.
Project Aim Statement
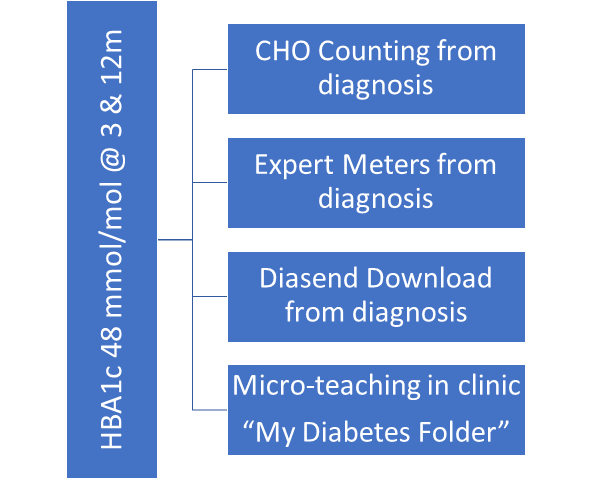
Our agreed aim was to achieve an HBA1c of 48 mmol/mol at 3 and 12 months post diagnosis.
Stakeholders
The Sheffield Children’s Diabetes Team is a large multi-disciplinary team including 4 consultant paediatricians, 2 paediatric doctors in training, 4 diabetes specialist nurses, 2 dieticians, 1 psychologist, 1 health care assistant and 1 administrator not all of whom work full-time or exclusively within the team.
Our patient population was specifically the newly diagnosed patients within our clinic but inevitably the changes in practice made will affect the entire clinic population over time.
PDSA Cycles / Solution(s) Tested
Plan:
To “brainstorm” the practicalities of the intervention, discuss with key stakeholders (nurse managers, ward staff including housekeepers, catering staff) and design resources for the ward staff to use. The dieticians to lead on upskilling ward staff to deliver basic carb counting to all ward staff.
Do:
The intervention to be implemented on December 1st 2017.
Study:
Data to be collected and displayed on run-charts:
- Time to first CHO counted meal (by diabetes team member)
- Number of CHO counted meals whilst in-patient (minimum 3)
- Length of hospital stay
- Average Blood Glucose at 7 and 30 days
- HBA1c at 3 and 12 months post diagnosis
Act:
Data to be reviewed at every fortnightly QI meeting and trends/outliers to be studied in depth and metrics added/removed as considered necessary by the team.
Data Results
Results Dec 2017-Sept 2018:

Live run charts of number of days from diagnosis to first carbohydrate counting with a member of the Diabetes Team, average blood glucose at 7 and 30 days post diagnosis, HBA1c at 3, 6 and 12 months are also being kept and are scrutinised at each QI meeting.
How This Improvement Will Be Sustained

Challenges and Learnings
As a team we have learned to be brave and fail fast. We are constantly reviewing progress and adapting the way we do things. The cohesion within the team and the relationship with the in-patient ward team (who had to be upskilled in carbohydrate counting and other aspects of diabetes management) has been massively improved. We have worked hard to publicise our QI initiatives within the Trust, locally, regionally and nationally and have kept our service users informed in clinic and via quarterly newsletters.
Our enthusiasm is infectious and team tenacity has improved. Excellent communication with all concerned is crucial and at times has been challenging but by improved transparency of our combined aim real progress has been made as seen in our improved HBA1c data.
Suggestions for Further Implementation
Having initiated carbohydrate counting from diagnosis over the past year we are continuing to educate ward staff on a rolling basis in order to embed this practice and have also started encouraging families to download their blood glucose results at home via Diasend from the time of diagnosis and all newly diagnosed patients are supplied with an expert meter.
We have implemented a programme of micro-teaching in clinic and are working on how best to evaluate this and work is also ongoing on the new “My Diabetes Folder” which will be a personalised resource for each child/young person to carry with them throughout their patient journey.
We have a number of other exciting ideas about possible next “chunks” to address via QI methodology but we are resisting the temptation to dilute the good work currently being done by attempting to do too many projects at once.
Project Lead: Dr Carrie MacKenzie
Organisation: Sheffield Children’s Diabetes Team
Published: May 2019
Hear Carrie reflect on her team’s journey throughout the QI Collaborative programme and offer recommendations to teams wishing to embark on quality improvement projects of their own, in Episode 1 of the Diabetes QI Collaborative podcasts.
