Using Two-Year Outcome Data to Drive Service Improvement for Preterm Infants in Bradford
This quality improvement project aimed to align with national standards and evaluate outcomes for neonatal care graduates, driving targeted service enhancements.
Authors
Dr Aishin Lok, Ceri Carless, Natalie Reynolds, Dr Kerry Blackett, and Dr Raj Lodh. Bradford Teaching Hospitals NHS Foundation Trust.
Background
Children born before 30 weeks’ gestation remain at high risk of long-term neurodevelopmental difficulties. To address this and ensure equitable, high-quality care, Bradford Neonatal Service launched a structured, consultant-led two-year follow-up programme in 2023. Bradford’s ethnically diverse and socio economically disadvantaged population presented additional challenges in implementing the NICE NG72 guideline.
Measures
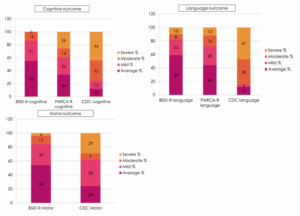
We evaluated follow-up quality by examining the proportion of children reviewed at two years’ corrected age, the assessment tools used, and compliance with NG72 developmental surveillance guidance and NNAP two-year follow-up indicators. Developmental outcomes were measured using the Bayley Scales of Infant and Toddler Development (Bayley- Revised (PARCA-R), and clinic records.
Improvement Plan
We used Plan Do Study Act (PDSA) cycles to strengthen follow-up processes and data quality.
• Cycle 1: Identified inconsistencies in outcome reporting. To improve reliability, we replaced postal PARCA-R questionnaires with digital links sent via text, introduced monthly Bayley-III clinics led by neonatologists and physiotherapists, and implemented consultant oversight of NNAP data entry to ensure accuracy.
• Cycle 2: Focused on integrating results. We combined Bayley-III (BSID III), PARCAR, and clinic records to build comprehensive developmental profiles, improving recognition of developmental delays and highlighting gaps in therapy access.
Outcomes
Between January 2022 and December 2024, 122 eligible infants reached their two years corrected age. 97.6% were reviewed at two years, a rate well above the national average. Bayley-III assessments were introduced in 2023; of the 122 children, 75 were evaluated, with 12 excluded as they were already under child development services (CDC). Paired Bayley and PARCA-R scores were available for 36 children. Combining all assessments, severe cognitive impairment was present in 18%, severe language impairment in 25%, and severe motor impairment in 14%. Speech and language delay emerged as the most frequent developmental concern. Overall, moderate-to-severe developmental delay affected nearly 45% of the cohort, based on Bayley-III assessments and clinical CDC reviews. Despite established referral pathways, service capacity for Speech and Language Therapy (SLT) remains insufficient.
Challenges and Learnings
Integrating data from multiple sources proved resource-intensive but was essential to building accurate developmental profiles. This highlighted the importance of streamlined systems for efficient follow-up. The most significant service gap was in Speech and Language Therapy (SLT), where demand consistently exceeded capacity. Limited access to timely SLT likely contributed to the high prevalence of language delay observed, underlining the need for expanded provision to meet the developmental needs of this high-risk group.
Future Plans
We plan to follow this cohort to school age, allowing comparison with Early Years Foundation Stage (EYFS) outcomes to better understand long-term trajectories. Expanding our database to include the most recent cohort will provide robust three-year outcome data. Incorporating demographic and equality variables such as ethnicity, deprivation, and primary language will help explore the influence of social factors on
outcomes. Benchmarking against national datasets will contextualise local results and guide targeted service development.
Top Tips For Implementation
Success in delivering a high-quality two-year follow-up service for children born at less than 30 weeks’ gestation depends on senior leadership backing, strong clinical leadership, and well-defined, structured pathways. Ongoing oversight of data qualityespecially ensuring accurate NNAP submissions is vital to inform local service
improvements and track progress against national standards. Multidisciplinary team engagement underpins consistency of care, while early collaboration with community and therapy services helps ensure timely interventions and smoother pathways for families.
Acknowledgements
We gratefully acknowledge the support and collaboration of the Bradford neonatal and paediatric neurodisability teams, therapy services, and the families who contributed to this project.
