Getting it Just Right: A QI Initiative in Preterm Thermoregulation
This QI project aimed to achieve ≥80% of babies (< 34 weeks gestation) to have a normothermic (36.5–37.5°C) admission temperature taken within one hour of birth.
Authors
Natasha G, Swati Jha, Enas Alyaldin, Adetokunbo Joacquim, Nupur Chauhan, Hasan Maldar, Sarah Green, Julia Arthur and Catriona Macdougall. Department of Neonatology, Addenbrooke’s Hospital, Cambridge University Hospitals NHS Foundation Trust.
Background
In 2022, our unit was identified as a negative outlier for the National Neonatal Audit Programme (NNAP) measure ‘Normal Temperature on Admission’, with only 59.2% of preterm babies <34 weeks achieving temperatures within the target range – well below the national average of 73.2% for that year.
Recognising the importance of thermoregulation in reducing preterm morbidity and mortality, we launched a targeted quality improvement initiative to address this. We engaged key stakeholders from members of the medical and nursing team to identify key challenges and potential solutions.
Measures
• Monthly prospective audits of normothermia rates in babies < 34 weeks gestation.
• Ongoing evaluation through PDSA cycles from December 2023 to March 2025
Our improvement plan:
In December 2023, we launched the “Think Temperature: Just Right” campaign. We focused on both data accuracy and clinical practice:
o Data integrity: Modified the EPIC–BadgerNet interface to ensure reliable temperature data transfer.
o Standardisation: Introduced a standardised approach to thermoregulation to prompt temperature checks and guide thermal care and a proforma to standardise documentation.
o Education: Delivered multidisciplinary education and simulation training.
o Iterative learning: Conducted prospective audits, and ‘deep dive’ into cases where compliance was not achieved to drive iterative changes. This identified issues with timely admissions in multiple births and hence repurposed a second transport
incubator to support this.
o Engagement: Shared learning via monthly updates and introduced a “Temperature Star of the Month” initiative to celebrate good practice.
Outcomes
Between December 2023 and March 2025, 225 babies <34 weeks were reviewed. Our median compliance with normothermia improved from 69.2% pre-intervention to 80.5% post-intervention.
A temporary dip in September 2024 during junior doctor changeover was quickly addressed with targeted education.
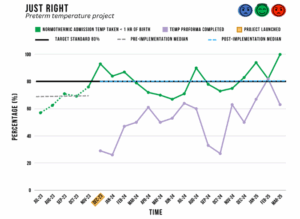
Figure 1. Run chart illustrating percentage of normothermic preterm babies <34 weeks’ gestation with admission
Challenges and learnings
• While proforma completion remains variable, we have since transitioned to an electronic version to improve uptake and consistency.
• A multi-faceted approach – combining system changes, education and culture building – has led to sustained improvements in thermal care within our unit.
Top tips for implementation
• Review data accuracy – ensure reliable, real time temperature data capture.
• Standardise approach – develop a clear protocol and/or proforma to guide thermal care and standardise documentation.
• Team engagement – regular communication, and celebrating good practice is important to build morale and maintain momentum.
• Adapt – use deep dives and PDSA cycles to ensure continual improvement.
Acknowledgements
Nil
