Driving Improvements in the Rates of Breast Feeding at Discharge from Neonatal Care
The neonatal team at Medway Maritime Hospital shares how national audit data has been used to drive improvements in the rates of breast feeding at discharge.
Background
The Oliver Fisher Neonatal Intensive Care Unit (NICU) is located within the Medway Maritime Hospital in Kent. Each year, around 1,000 babies spend some time being looked after in the unit as they need intensive, high dependency, transitional or special care. The unit is located within the wider South East Coast Neonatal Operational Delivery Network (ODN).
The Oliver Fisher NICU has participated in the National Neonatal Audit Programme (NNAP) since 2007 with audit results for the unit consistently confirming high standards of care. The 2015 report on 2014 data however showed a drop in our rates of breast milk feeding at discharge. Furthermore, and for the first time ever, we were identified as a low outlier for this NNAP audit measure with breast feeding rates at discharge of 34% compared to the national average of 60% in babies born at less than 33 weeks gestation.
In this case study we highlight that with a quality improvement approach, and simple but focused interventions, we have been able to achieve a significant improvement in breast milk feeding rates over a relatively short period of time.
The following table shows the 2014 results for the Oliver Fisher NICU for the NNAP audit measure which asked: “What proportion of babies born at less than 33 weeks gestation were receiving any of their own mother’s milk at discharge to home from the neonatal unit?”. Results for the unit are shown against those for both the National and South East Coast Neonatal Network averages for the same year:
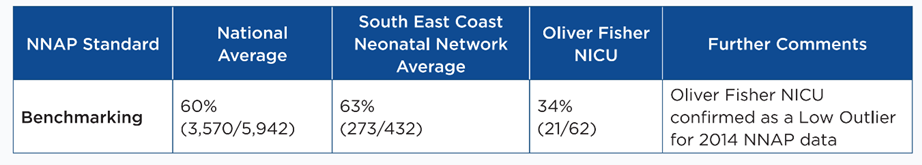
We were notified about our provisional low outlier status for this audit measure by the NNAP clinical lead in May 2015 and we received formal confirmation of the low outlier status in October 2015 prior to the launch of the annual report in November 2015.
What we did in response to our low outlier status
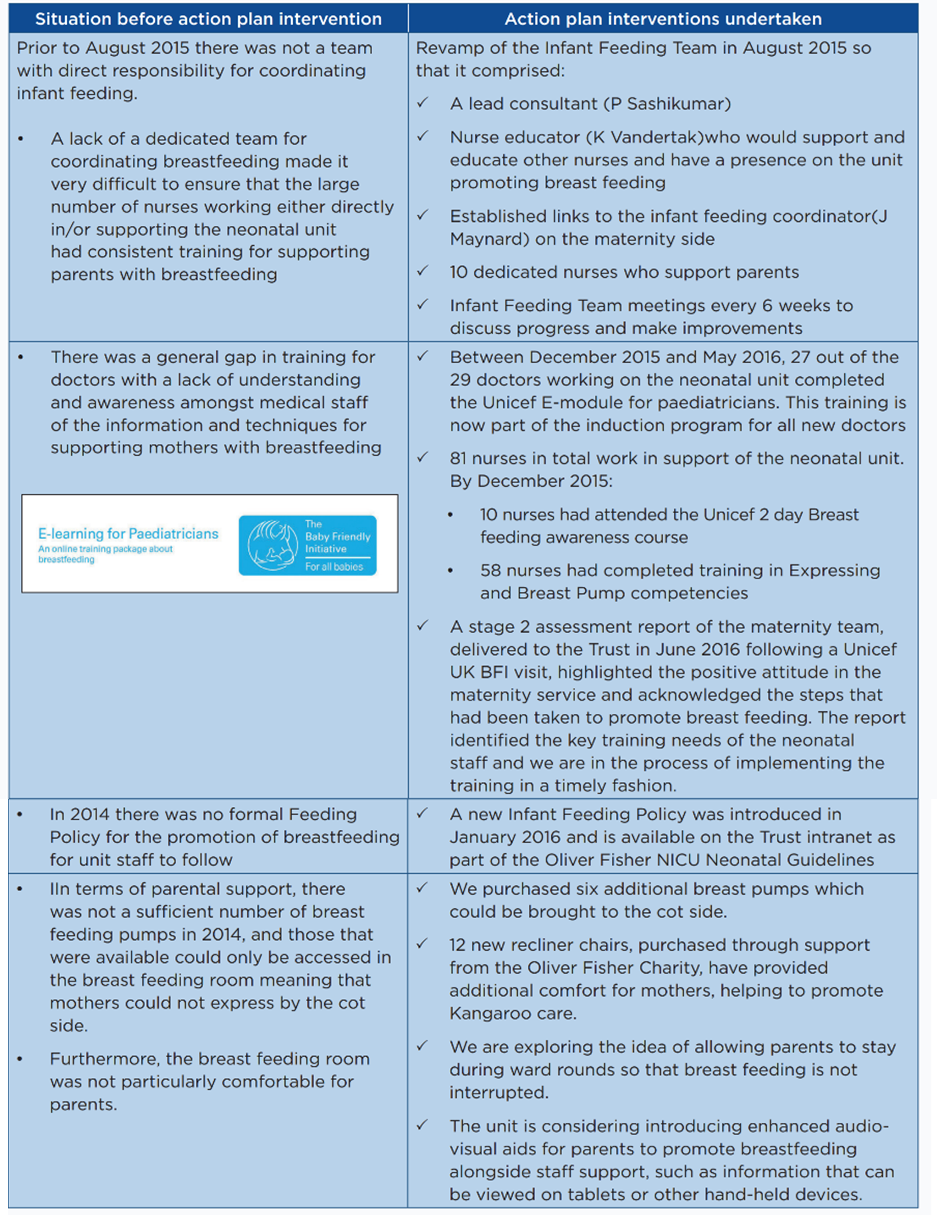
We developed a quality improvement action plan which included the revamping of the Infant Feeding Team and a comprehensive review our existing breast feeding practice. The team implemented the elements of the agreed action plan and made small and steady progress to improve the awareness among the staff of how to provide effective support for breast feeding. The team worked very closely with the midwifery team in the hospital and in the community to provide coordinated support for families.
What we have achieved
By undertaking quality improvement activities we believe that we have made significant improvements in our breast feeding support for families and in our adherence to the NNAP standard for this aspect of neonatal care. The NNAP provides all units that participate in the audit with quarterly reports which show unit performance against the NNAP audit measures.
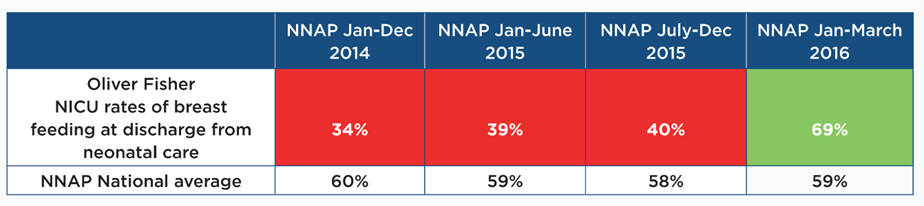
The latest report, which covered the period 1 January to 30 June 2016, validated these improvements by showing breast feeding rates for our unit of 69%, a vast improvement on the situation in 2014 as detailed below – figures highlighted in red are below the NNAP national average and those in green are above the national average:
When thinking about safety, clinical effectiveness, efficiency and/or responsiveness, we believe that by following a defined quality improvement plan we have improved patient care and experience in the following areas:
- Increased breast milk feeding rates for high risk Preterm Infants.
- Improved NNAP performance from low outlier status in 2014 to above the national average by mid-2016.
- Provided levels of care and support which should improve patient outcomes.
- Working towards achieving UNICEF UK Baby Friendly Accreditation.
Acknowledgements
- Infant feeding team, Oliver Fisher Neonatal Unit
- Oliver Fisher Neonatal Unit Staff
Download the full NNAP case study including the local neonatal nursing guidelines feeding policy for breast feeding and breast milk developed by the team here.
Authors: Dr P Sashikumar (Consultant Neonatologist), K. Vandertak (Nurse Educator, Neonatal Infant Feeding Team), L.Proffitt (Neonatal Matron), S Jones (Advanced Neonatal Nurse Practitioner).
Organisation: Medway Maritime Hospital, Medway NHS Foundation Trust
Originally published in the 2016 NNAP Annual Report.
