Keeping Mothers & Babies Together: Getting It Right First Time
Introducing a 'Keeping Mothers and Babies Together' pathway at the Royal Free London NHS Foundation Trust to reduce neonatal admissions to 6% and create a single unified pathway of care for all ‘at risk’ infants.
Background
The ‘Atain’ (avoiding term admissions into neonatal units) programme aims to address rising term (≥37+0 weeks) admissions by identifying the main reasons for admissions (respiratory conditions, hypoglycaemia, jaundice, asphyxia). Observation of the clinical journey for infants with risk factors for postnatal compromise (‘at-risk’ infants) highlights the complex pathways our teams were navigating.
Clinical guidelines differed according to the specific risk factor in frequency and length of observations and support offered leading to variation in care delivery. This extended to the management of late preterm (34+0-36+6 weeks) infants who were often pre-emptively separated from their mothers. Parent diaries highlighted how disempowered and vulnerable they felt in looking after their ‘at-risk’ baby. The need for standardisation and simplification was clear.
Aim
We extended the National Neonatal Audit Programme (NNAP) measure to minimise inappropriate separation of mothers and term babies to include both term and late preterm infants and aimed to reduce neonatal admissions to 6% by creating a single unified pathway of care for all ‘at risk’ infants.
Our improvement plan
The traditional approaches of focusing on individual risk factors fail to address the underlying drivers of unwarranted variation in care delivery. The Royal Free Keeping Mothers and Babies Together (KMB2) pathway centres on standardising care through the introduction of a single, simplified pathway focussing on the following key elements:
- Standardised assessment of early respiratory distress
- First hour care bundle
- Orange ‘hat-risk’ nudge
- Unified observation regime for all at-risk infants and revised Newborn Early Warning Trigger Tool (NEWTT) chart
- Written information for families.
We started by devising a unified observation regime. Each step was tested, revised using rapid plan-do- study-act (PDSA) cycles and embedded before incremental introduction of another facet of the pathway. Collaboration with families and staff has been central in producing the pathway. The pathway team includes a father. Focus groups, one-to-one interviews and video feedback were used to inform the development of the pathway documents and continued to ensure rapid revision and retesting to hone the accessibility and utility of the pathway.
Measures and outcomes
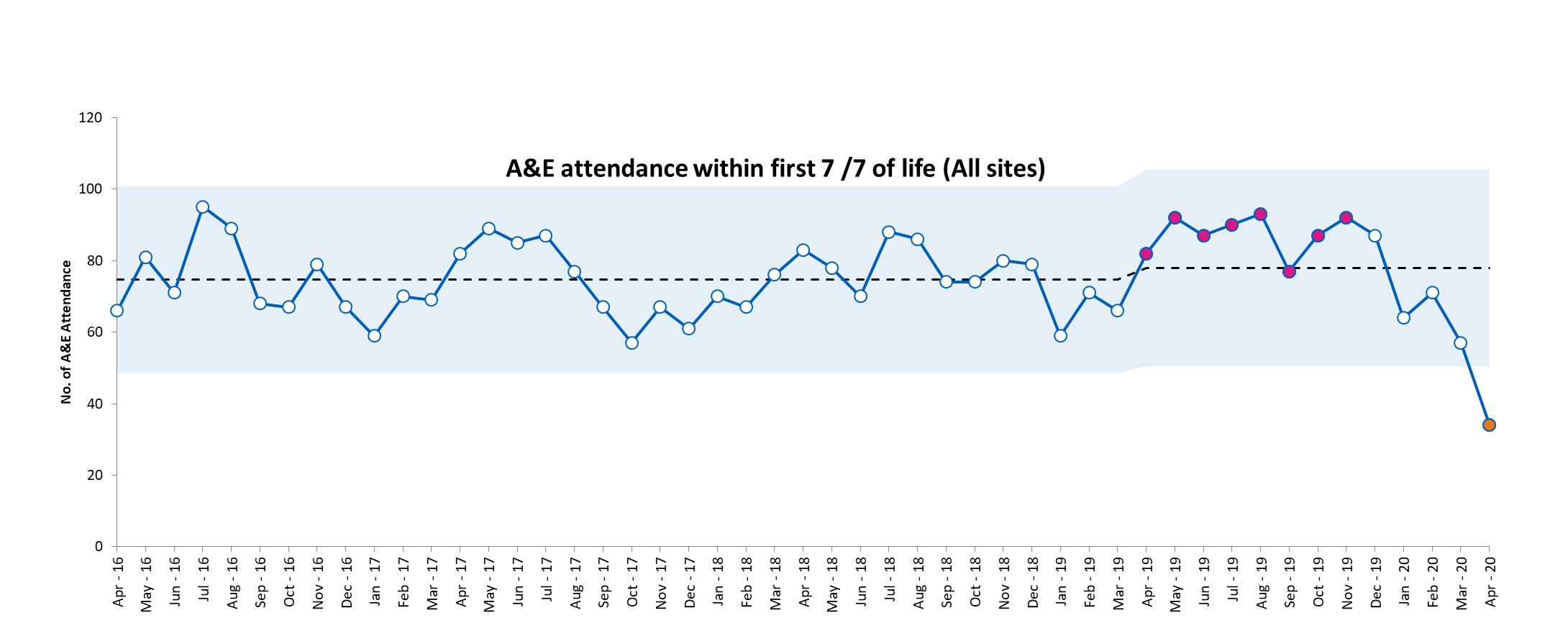
The baseline admission rate for infants born after 34 completed weeks gestation was 8.3%. We reduced this to 6.7% over a 2year period (November 2017-November 2019). We continue to work towards achieving our target of 6%. Each PDSA cycle was tested using both qualitative (questionnaires, focus groups and interviews) and quantitative (eg number and quality of NEWTT charts and first hour care bundles being completed and obstacles to this) process measures. These measures were used to revise each step. Balancing measures included length of stay of mothers on the postnatal wards and presentation or readmission through accident & emergency departments within 7 days of birth. Both of these measures remained unchanged indicating that these infants are being safely transitioned home.

Sustainability
Sustainability has been primarily achieved by involving frontline staff in designing, refining and implementing the pathway and ensuring we achieved our brief of simplifying the process. During the implementation phase, the Trust introduced electronic patient records (EPR). We digitalised the pathway within the EPR to support sustainability and our midwifery team have welcomed this introduction reporting it was “straight forward…makes sense.”.
Challenges and learning
We initially tried to implement the whole pathway at once which resulted in staff rejecting it as too complex. Implementing a single aspect of the pathway, with rapid revision and refinement based on staff and parent feedback, proved more successful. Challenging preconceptions was difficult. Taking the lead from Richard Thaler’s Nudge theory, we wanted to introduce orange hats for ‘at risk’ infants so they can be easily identified on a busy postnatal ward as requiring extra observations and feeding and temperature support. Staff were concerned that families would feel stigmatised. Parents were overwhelmingly enthusiastic citing increased confidence to ask for the extra support they needed. Hearing this directly from parents led to rapid adoption.
Top tips for implementation
- It was important that the vision was clear and the name of the project was chosen to reflect this. One parent commented, “the name of the pathway…really captured what it was setting out to do”.
- Engagement with all members of the team was crucial. Using a variety of feedback methods ensured a wide reach.
- The role of the parent voice cannot be underestimated.
- Communication within and across our teams has been important. Involving all the team by actively seeking feedback and acting on it brought a whole team ethos to this work.
- Board level support was important in terms of support offered but also in recognising and celebrating our successes.
- Spreading learning is important to ensure other teams were not reinventing the wheel. We have presented the KMB2 pathway at national and international conferences, through medical literature and shared widely through social media (our Twitter handle is @MumBaby2gether). The pathway (in whole or aspects) has been adopted by Trusts across the UK and is available to all NHS Trusts via the NHS Improvement hub.
Acknowledgements
The maternity and neonatal teams at both Barnet and Royal Free Hospitals have positively embraced the KMB2 pathway. Their energy, drive and passion has been matched by the families who have contributed to producing this pathway.
Authors: Shanthi Shanmugalingam, Lorraine Gallagher, and Rose Villar
Organisation: Royal Free London NHS Foundation Trust
First published in the NNAP Annual Report 2020
