Use of non-synchronised non-invasive positive pressure ventilation (NS-NIPPV) to reduce extubation failure in preterm infants
This QI project aimed to use NIPPV as a mode of extubation for all preterm infants born at <28 weeks’ gestation and for all high-risk infants <32 weeks gestation.
Publication date: 12 October 2023
Authors
Dr Amitava Sur, Dr Anshuman Paria & Dr Adarsh Bhulani – Neonatal consultants, Lancashire Women and Newborn Centre
Background
The primary driver behind this focused Quality Improvement (QI) initiative was the higher than national incidence of bronchopulmonary dysplasia (BPD) in the Lancashire Women and Newborn Centre. The incidence as reported by the National Neonatal Audit Programme (NNAP) annual reports was 50.8% in 2020 & 47% in 2021 (the national mean incidence of BPD for 2021 was 31%).
Three areas of improvement were identified and process mapped according to the preterm infant’s journey through the neonatal unit. These were delivery room interventions (perinatal and immediate stabilisation), early neonatal respiratory practices and minimising lung injury in the evolving phase. This initiative was part of the early respiratory optimisation process in the neonatal unit. It was identified that in 2019, almost 50% of preterm infants failed extubation at first attempt in our unit. The modalities used for extubation were variable; either continuous positive airway pressure (CPAP) through infant flow driver or high-flow nasal cannula (HFNC). These are limited by fixed upper limits of flow delivery. Hence, there was an inability to consistently delivery higher positive end expiratory pressure (PEEP)/ mean airway pressure (MAP).
Rationale for change
Single centre cohorts and large study groups have reported extubation failures to be independently associated with higher adjusted rates of BPD and mortality. The secondary analysis of infants enrolled in the SUPPORT trial1 reported a three times higher risk of BPD in infants who failed extubation.
Emerging moderate to high-quality evidence has concluded that when compared to CPAP or HFNC, both synchronised and non-synchronised NIPPV are more successful in preventing extubation failures.2, 3
Project aim
To use NIPPV as a mode of extubation for all preterm infants born at <28 weeks’ gestation and for all high-risk infants <32 weeks gestation.
Stakeholders
Consultant lead(s), nursing educators and senior nursing staff, advanced nurse practitioner lead (ANNP).
Measures
- Extubation failure rates (defined as a need for mechanical ventilation within 72 hours after extubation) were analysed with other associated factors, such as:ventilation settings prior to extubation, day of life when extubation was attempted first and demographics.
- Three separate internal audit cycles were carried out and data was analysed.
Improvement plan
- NS-NIPPV delivered by ventilator (Draeger Vn 500) was introduced as extubation support in 2019. Its use for early extubation was ad-hoc throughout 2019.
- From 2020, all preterm infants <28 weeks and high risk <32 weeks were extubated to NS-NIPPV or high CPAP (8 cm H20) via ventilator as protocol (<28 weeks exclusively extubated to NS-NIPPV).
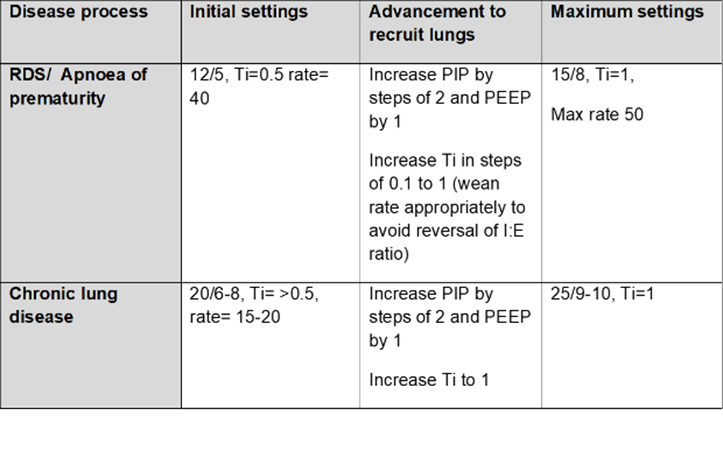
- A protocolised algorithm was developed for peri-extubation practices (Figure 1) and an NIPPV guideline was developed for clinical use based on available evidence and literature (Figure 2).
Figure 1: Extubation checklist and timeline, Lancashire Women & Newborn Centre
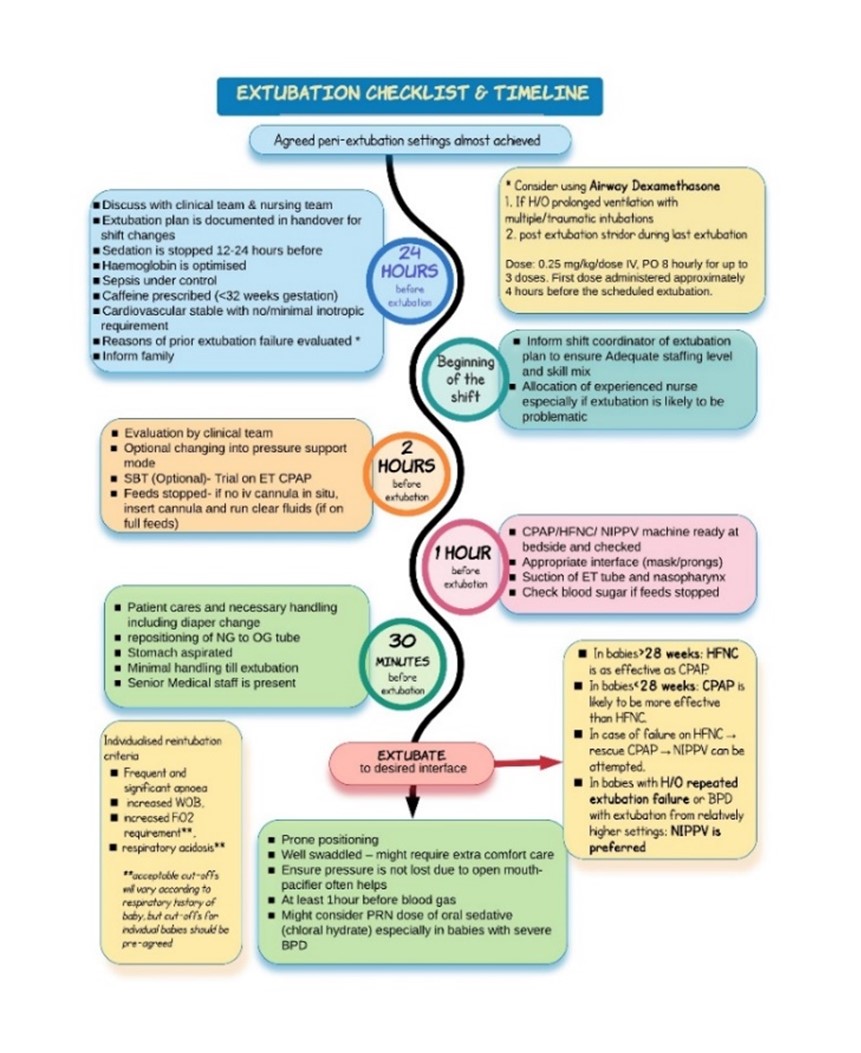
Figure 2: NIPPV guideline, Lancashire Women and Newborn Centre
Challenges
The predominant challenges were around the shift associated with change from a long-sustained practice and hesitation with using higher post-extubation pressure. Other challenges included equipment familiarity, consumables and overall engagement.
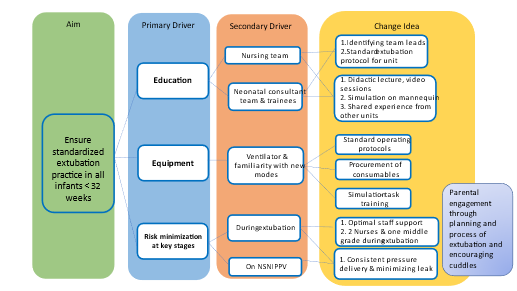
These were addressed through: short educational sessions on the physiological rationale, sharing experience from other units using NIPPV and multiple simulation sessions using task training methods with mannequins. Videos were developed and disseminated for training. (Driver diagram- Figure 3)
Two neonatal consultants, two nursing educators and one ANNP were identified as leads for this project.
Figure 3: Driver diagram, ensuring standardised extubation practice
Outcomes
- Failure rates showed a significant and sustained reduction from 72% (2017) to 50% (2019) reaching a nadir of 27% (2020)
- For 2022, we looked specifically at infants born <28 weeks and extubation success in the first 14 days of life. 44 infants were born <28 weeks, of whom 1 was transferred out within the first 24 hours. Of the remaining 43 infants: 2 did not require mechanical ventilation(4.7%), 18 (41.8%) were extubated within the first 14 days of life and 23 (53.5%) were not extubated in the first 14 days.
- Among the 18 who were extubated, 15 (83%) were successful. The mean gestational age was 26.7 weeks. 14 of them were extubated to NS-NIPPV or ventilator driven CPAP. 1 was extubated directly to HFNC.
- The unit has also reported a parallel and consistent reduction in incidence of BPD, although we have still not been able to reach the national average (34% in Q3 2021-22 , 26.7% in Q4 2021-22 and 32.3 in Q1 2022-23 ).
Culture change
- Consistent and sustained improvement was observed in staff engagement. This has now been embedded in practice with nursing members independently extubating to NIPPV when a decision has been made on rounds.
- Successful use of NS-NIPPV has also enabled and empowered the team to confidently extubate early.
Lessons learnt
Culture shift: The main challenge for implementation and change in practice, was familiarity and confidence of staff with a new modality and uncertainty around the practice essentials. It helped to provide focused training on equipment in addition to developing a unit guideline based on available evidence, to use as a template.
Equipment and interface: Nasal bridge injury was an encountered problem in the extremely preterm infants. We have a standard protocol of alternating between prongs and masks every 4 to6, hours to minimise this.
The model of interfaces we use has provision for “extra small prongs” but only “small” sized masks. We have encountered scenarios, especially in the smallest infants, where we could not find a mask size small enough and prongs were not well tolerated.
Extubation awareness: Another area of improvement is the focus and awareness for early extubation. We are trying to increase awareness; that during every clinical round or assessment, irrespective of time of day, it should be questioned whether an infant needs to remain ventilated. The success of extubation is a combined effort of clinical pragmatism, optimising the extubation environment and skilled nursing care.
Top tips for implementation
- Evidence is a powerful tool. When evidence is presented in a manner which is relatable to all members of staff, it can influence major changes in attitude and practice. The evidence behind use of NS-NIPPV or S-NIPPV is emerging and growing stronger.
- Good background data analysis to identify gaps and areas for improvement makes a strong case for QI.
- Not being afraid to use higher CPAP pressures or aim for a MAP of 8 or above when using NS-NIPPV in the post extubation period can prevent post-extubation atelectasis.
- Having a standardised extubation algorithm and checklist, although not strictly evidence-based, is a good practice.
Acknowledgements
Nursing education team at Lancashire Women and Newborn Centre
References
Chawla S, Natarajan G, Shankaran S, Carper B, Brion LP, Keszler M, et al. Markers of Successful Extubation in Extremely Preterm Infants, and Morbidity After Failed Extubation. J Pediatr. 2017 Oct;189:113-119.e2.
Lemyre B, Davis PG, De Paoli AG, Kirpalani H. Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for preterm neonates after extubation. Cochrane Database of Systematic Reviews. 2017 Feb 1;2017(2).
Ramaswamy VV, More K, Roehr CC, Bandiya P, Nangia S. Efficacy of noninvasive respiratory support modes for primary respiratory support in preterm neonates with respiratory distress syndrome: Systematic review and network meta‐analysis. Pediatr Pulmonol. 2020 Nov 4;55(11):2940–63.
