Optimising Early Maternal Breast Milk (MBM) for Preterm Infants
Supporting the implementation of the five Perinatal Core Elements to optimise early MBM for preterm babies across the St Mary’s Hospital Managed Clinical Service at Manchester University NHS Foundation Trust
Background
The QI project started in December 2020 with establishing a multidisciplinary working group of staff across the St Mary’s Hospital Managed Clinical Service (MCS) inclusive of representatives from the Neonatal Units, Maternity and Postnatal Wards. Focus was placed on the following challenges:
- Named equipment checker for both Newborn Services and Maternity
- Education for parents and staff
- Enhancing parental involvement in this initiative
In the North West of England, achieving high rates of breastmilk provision has been challenging, with St Mary’s Hospital’s NNAP results as below:
- 2018 – 47% babies <33/40 receiving mother’s own milk (MOM) at discharge (national average 60%)
- 2019 – 43% babies <33/40 receiving MOM at discharge (national average 58%)
- 2020 – 61.5% babies <32/40 receiving MOM at discharge (national average 60%)
- 2020 –76.6% babies <32/40 receiving MOM at 14 days old (national average 82%)
In response to serially disappointing results, the key focus of the QI project was supporting the implementation of the five Perinatal Core Elements to optimise early MBM for preterm babies (BAPM 2020).
In the NICU, these two elements were concentrated on:
- Initiation of expressing soon after birth (aim within 2 hours) with easy access to support, training and equipment
- Early colostrum (ideally within 6 hours of birth and within 24 hours) to be the first enteral feed given to baby
Improvement plan
The project recognised the need to increase the availability of MBM within 24 hours, to ensure that MBM is available at day 14 and to enhance breastfeeding rates at discharge. Further to this, the project’s main aims were:
- To achieve staff consistency in information delivery to mothers across Newborn Services and Maternity
- To increase staff awareness of the benefits of early breast milk
- To improve the quality of information provided to parents about all aspects of expressing
- To drive to improve standards of breastmilk administration from within 6 hours of birth to within 2 hours, with a new expressing method of hand massage, double electric pumping then hand expressing
- To increase Maternity and Inreach pump training and availability
- To provide refreshers on staff training and refocus on establishing Feeding Champions
- To rebrand breastmilk, expressing and feeding under a ‘Golden Drops’ umbrella
Outcomes
The NNAP 2020 report shows that we had 76.6% babies <32/40 receiving MOM at 14 days old (national average 82%) while our predicted data for 2021 so far shows a mean of 77.3%. While this seems like a modest improvement, our monthly figures are promising for gradual sustained change.
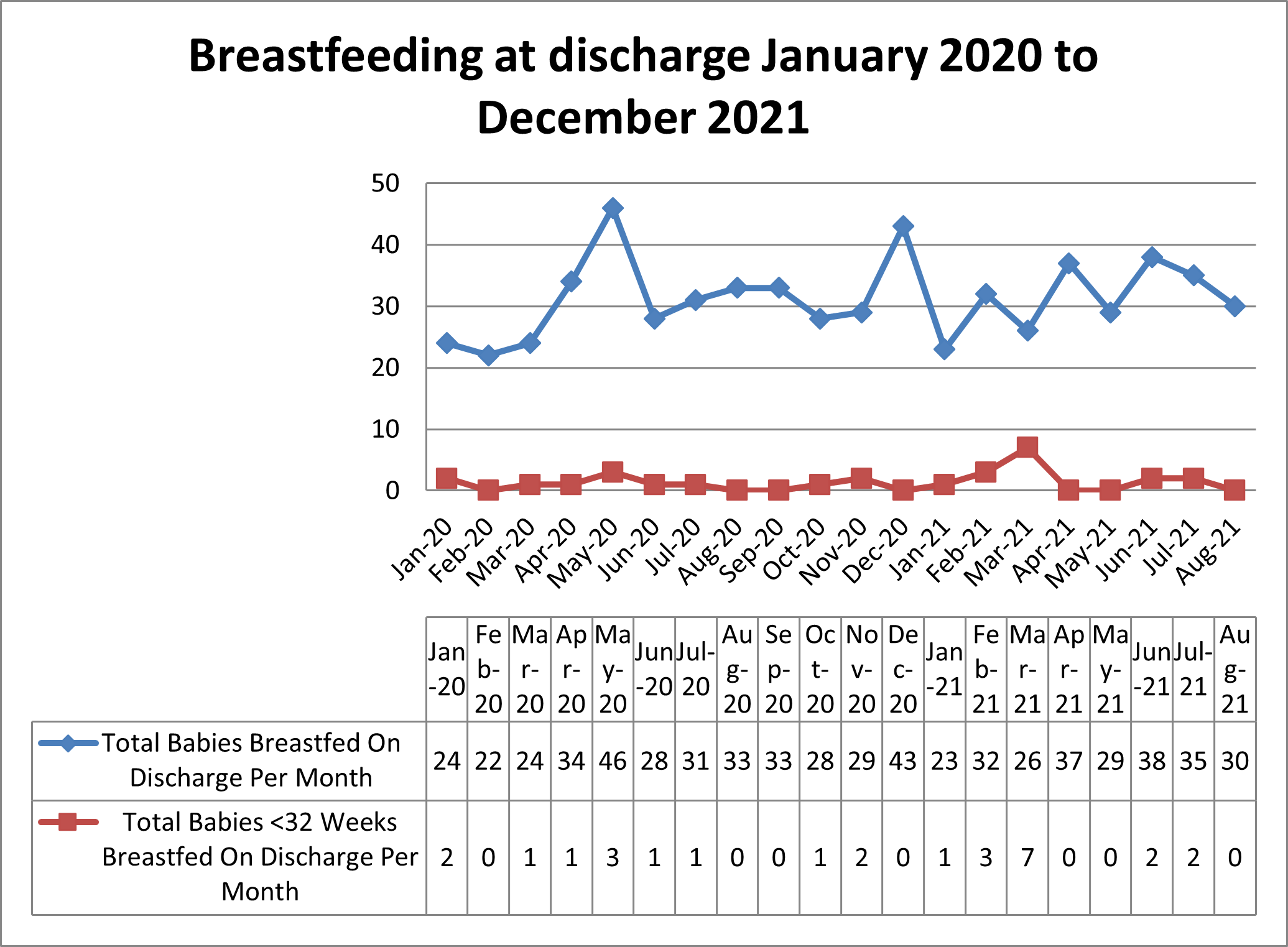
In 2020 we had 61.5% babies <32/40 receiving MOM at discharge (national average 60%) but now increased to a mean of 67.2%, which we are delighted with. The run-chart below illustrates this improvement:
Top tips for implementation
We feel that more Infant Feeding champions, funding, and time allocated to the quality improvement programme would have a significant effect on breastfeeding outcomes and will continue to seek ways to facilitate this.
Authors: C. White, P. Colwell, M. Hutchison-Saxon, A. O’ Doherty, K. Eaton, R. Gottstein, K Munthali, N. Edi-Osagie and K. Tanney
Organisation: Newborn Intensive Care Unit, Saint Mary’s Hospital, Manchester University NHS Foundation Trust (MFT)
Published as part of the NNAP Annual Report on 2020 data
