Deferred Cord Clamping in Preterm Infants
Improvement projects from Sheffield Teaching Hospitals, Ashford and St Peter's Hospitals, and York and Scarborough Teaching Hospitals NHS Foundation Trusts focussed on the implementation of deferred cord clamping as per national guidance.
Improving rates of deferred cord clamping for neonates born at less than 34 weeks gestation in a tertiary neonatal unit
Jessop Wing Neonatal Intensive Care Unit, Sheffield Teaching Hospitals NHS Foundation Trust
Background
Deferred cord clamping (DCC) has a growing evidence base demonstrating positive impact on neonatal morbidity and mortality. Despite the evidence base the Jessop Wing was found to have the lowest rates of DCC for babies born at less than 34 weeks within the region. Initial rates of DCC were 18% for preterm babies. In response to this data work was undertaken to review practice and implement change to improve rates of DCC within the unit.
Stakeholders for this project included patients and their parents, organisational heads of department and the wider neonatal network to optimise the care provided for preterm neonates. Initial literature search was completed as part of the MatNeo Safety Collaborative with NHS Improvement.
Measures
Initial data collection looked at practices prior to commencement of DCC QI project aiming to identify barriers to babies receiving DCC. An extensive literature search was undertaken alongside collaboration with other local and national units to develop a guideline for DCC.
A series of PDSA cycles were used to evaluate the implementation of the guideline within the unit. Various strategies were trialled to further improve rates of DCC including observation of practices at another tertiary unit with higher rates of DCC and the introduction of two LifeStart™1 trolleys to facilitate DCC.
Training on the use of the LifeStart™ trolley was provided for all nursing staff and included in doctor induction at each new rotation. In addition, regular multi-disciplinary simulation training (neonatal staff and midwives) was utilised to improve familiarity with equipment and provide the opportunity for troubleshooting. Posters were placed on routes to labour ward and obstetric theatres to remind staff attending deliveries. A change in practice to resuscitate newborns in theatres also occurred to facilitate more effective DCC.
PDSA cycles are ongoing to monitor rates, provide feedback to staff and continue to implement change where necessary.
Our improvement plan
This quality improvement project aimed to improve rates of DCC within the Jessop Wing Neonatal Intensive Care Unit. Barriers were identified, change implemented (development of a guideline, purchase of 2 LifeStart™ trolleys and training for medical and nursing staff) and data collected to monitor rates. Results were calculated monthly and disseminated to staff with collated data and review every 6 months at the unit audit meeting.
The aim was to provide deferred cord clamping for all eligible babies born at the Jessop Wing NICU at less than 34 weeks gestation, improve rates and maintain improved standards. The project was evaluated by prospective audit with ongoing data collection.
Barriers preventing DCC were identified. They included lack of knowledge and awareness of the practice and its benefits, lack of equipment to facilitate DCC whilst maintaining thermoregulation and absence of a guideline to standardise procedures.
Outcomes
Initial rates of DCC for premature neonates born at the Jessop Wing in 2018 were just 18% which was far lower than other tertiary units within the Yorkshire and Humber region. This figure rose to 66% by the end of the initial 6 months. LifeStart™ trolley routine use was initiated following the first 6 months of data collection with training for medical and nursing staff on this equipment.
Throughout the last 6 months of data collection, rates of DCC for all babies born before 33 weeks gestation have been between 47-100%. The results stated include all babies delivered including those with contraindications according to local guidance due to a lack of universal recognition of babies eligible for DCC – see table below for results:
| Month | Number of babies born </=32/40 | Number of babies in whom DCC was considered inappropriate under local guidance | Number of babies received 60s or more DCC |
| March 2021 | 7 | 1 | 4 (57%) |
| April 2021 | 15 | 5 | 7 (47%) |
| May 2021 | 4 | 0 | 4 (100%) |
| June 2021 | 13 | 5 | 7 (54%) |
| July 2021 | 15 | 2 | 10 (67%) |
| August 2021 | 11 | 2 | 6 (54%) |
The Jessop Wing guideline for DCC has been updated to include new eligibility criteria. DCC and LifeStart™ training is included has been incorporated in induction and regular in situ simulation. Simulation has developed to become multidisciplinary including midwifery staff. This means simulation is more realistic and all staff attending preterm deliveries are familiar with the equipment used and the process of DCC. There is increased awareness of DCC practices with posters displayed throughout the neonatal unit, labour ward, and obstetric theatres.
Implementation of DCC has increased multidisciplinary communication and planning in general as well as in planning for DCC. DCC is specifically mentioned on PREM delivery forms used at this neonatal unit during preterm deliveries. Doctors completing the document are encouraged to plan for/discuss DCC with parents during antenatal counselling, prompted to discuss this at a pre-delivery MDT huddle and document DCC contemporaneously – by planning thoroughly for DCC the opportunity is maximised.
The success of this project is largely due to the sharing of information and teaching of new techniques within the unit and the wider multidisciplinary team. Providing more opportunities to practice skills and increase familiarity with processes has contributed to a sustained increase in DCC rates.
Repetition of the PDSA cycle regularly monitors progress and identifies areas for continuing development. On-going audit and review of data with feedback from staff will be used to monitor DCC rates and implement changes as required. Recently, a new breathing circuit with longer length has been introduced which may offer an alternative to the LifeStart™ for labour ward. This will be alongside continued education and simulation which also provide opportunities to identify barriers and issues in practice.
Further quality improvement work on DCC will look at sustaining improvement in rates of DCC at this tertiary neonatal unit with DCC for all eligible preterm babies being the gold standard. Ongoing suggestions for work in this area include facilitating parental touch and intact cord stabilisation processes.
Challenges and learnings
The initial challenge of this project was developing and cascading of an evidence-based guideline to standardise the process within the neonatal unit. The initial process involved movement of the resuscitaire to the mother’s bedside to ensure there was due consideration of thermoregulation during the DCC process. This process was taught to the neonatal staff but also required dissemination to the maternity and obstetric teams which was challenging due to numbers and shift patterns. Audit data collected from this initial stage showed barriers such as space within the delivery room as a barrier to providing DCC.
Following the arrival of the LifeStart™ trolleys the process again required teaching to members of the neonatal team both medical and nursing. This provided some challenges due to shift patterns and availability of those familiar with the equipment to teach. It was felt by some staff members that a single session was not enough to become confident in using the equipment so more regular training sessions were made available alongside the simulation programme.
When neonatal staff were relocated into theatres for deliveries there was training for scrub nurses to drape the LifeStart™ trolley to maintain sterility. The COVID-19 pandemic affected work on DCC particularly in theatres as the neonatal team returned to the separate resuscitation room for social distancing reasons. This meant that the decision for DCC in theatres was made by the obstetric team. When guidance allowed, the neonatal team moved back into theatres for deliveries.
Other barriers identified from the audit included lack of time to set up equipment, lack of space within the delivery room and the umbilical cord being too short to reach the LifeStart trolley.
Top tips for implementation
This quality improvement project could be implemented throughout the region to all units caring for preterm neonates. Data has been shared with the Neonatal ODN to support development in other units. The development of a guideline for deferred cord clamping within the local unit is an excellent starting point alongside educational session highlighting the importance of DCC and the impact on mortality and morbidity. Data can be easily collected by doctors attending deliveries or from looking at Badger information. Liaison with other units within the region and nationally will help to support implementation.
Authors: Myers L., Reeks, L., Williams, T., Wilson, L., Dockery, M., Salvanos, J., Sherwood, E., Smith, C.
Implementation of delayed cord clamping in all preterm infants
St Peter’s Neonatal Unit, Ashford and St Peter’s Hospitals NHS Foundation Trust
Background
Prior to 2019, we were practising umbilical cord milking (UCM) in all preterm infants in our unit. With increasing evidence on physiological DCC being the best method for optimal cord management (OCM), we wanted to change our practice from UCM to DCC. We started this quality improvement project (QIP) in June 2019. Soon afterwards the NNAP introduced DCC as a new pilot measure for 2020. This allowed us to focus more on this QIP over the next 18 months to slowly improve our rates of DCC.
As per the latest BAPM guidance, DCC for at least 1 minute is the preferred method of OCM in preterm infants. Our aim was to introduce this alongside respiratory stabilisation using high flow nasal cannula oxygen (HFNC). We aimed to facilitate preterm babies to have physiological transition of breathing established over 1-3 minutes before cord clamping called the new ‘ABC’ approach – airway patient, breathing established and then cord clamping to be done, ideally after 3 minutes.
The new BAPM toolkit on OCM published in December 2020 was very helpful to further the engagement of all staff members.
In addition to introducing a new practice, we faced resistance due to a need to change our practice from UCM to DCC. This needed a multi-disciplinary team approach between maternity, neonatal and theatre staff and a number of ongoing audit cycles using NNAP data to achieve our aims.
Our primary aim was to change our practice from UCM to DCC for all preterm infants.
Our secondary aims were:
- To continue to provide non-invasive respiratory stabilisation at birth using mobile HFNC oxygen as needed
- To continue to promote and maintain normothermia while implementing DCC
- To implement delivery room cuddle (DRC) for babies with parents
- To ensure that DCC and DRC do not result in a delay in admission and influence normoglycemia at admission
Measures
We started implementing this change in November 2019, initially with an aim to implement a minimum of 30 seconds of DCC to promote team confidence with this change in practice. We were achieving around 60 -70% success rates for DCC in our first PDSA cycle from November 2019 to February 2020.
We reviewed the cases and identified common themes for failure to implement DCC and addressed them in the next 6 months. These included poor communication between team members; lack of confidence if the baby wasn’t breathing/looked pale; equipment issues and special circumstances like monochorionic twins. We set out clear roles/responsibilities for each team member to communicate well, provided more training through simulation and by having an additional competent senior member attending the extreme preterm delivery to support DCC, and updating the guidelines to support DCC in monochorionic twins. We also shared our data regularly through monthly newsletters.
In the next PDSA cycle between March-August 2020, we noted that our rates of DCC were fluctuating on and off and that new members of the team had limited training. So, we incorporated a mandatory 1 hr session for doctors’ induction every 6 months. Furthermore, to help with consistent training, we produced 2 training videos to be shown to all new staff, and for regular training updates. We also introduced a new pack with all consumables needed for initial stabilisation for the first 5 minutes which facilitated equipment preparation. Additionally, we streamlined the equipment checking process for every shift, to ensure it was always ready.
In the final PDSA cycle from September 2020 to February 2021, we worked to introduce a new preterm birth checklist to be used by midwives and a new parent information leaflet to be given to all parents at booking to inform them of the benefits of DCC. Finally, we have seen that our rates of DCC remained consistently >90%. This also coincided with the release of BAPM toolkit which helped obstetricians and midwives to engage further.
We are working to embed these changes in our ongoing practice and continue to audit our rates using NNAP data.
Our improvement plan
We planned to measure the improvement through regular PDSA cycles every 4-6 months using the NNAP data set on DCC and temperature at birth. We also used an updated neonatal stabilisation sheet to capture additional data to evaluate the mode of respiratory stabilisation, rates of DRC and blood sugar monitoring at admission.
We set up a neonatal team of doctors and nurses with a lead consultant to kick start the project. We also had support from Inspiration Healthcare, UK, as they provided us with a purpose-built stabilisation platform called LifeStart™ on loan to do simulations over a period of 4 months to trial the equipment. Following implementing the practice, we worked closely with the midwifery team, obstetricians, and theatre staff to set up an MDT approach. Our neonatal unit charity fund supported us with the cost of buying the LifeStart™ and other accessories needed to provide DCC.
Outcomes
The project successfully changed the practice from UCM to DCC to optimise the cord management at birth in all preterm infants. Slowly and steadily we were able to address the barriers to changes with this QIP. The graph below shows the results of this QIP since August 2019.
Rates of implementation of DCC:

In the first 12 months, we were able to achieve an average of 75% of implementation rates every month. However, with the launch of the BAPM toolkit, we were able to push the focus more, especially amongst the obstetricians and midwifery staff. The BAPM toolkit also provided guidance on special circumstances like management of a short cord, twins, and placental abruption.
Since February 2021, we improved our average rates of DCC implementation from 75% to 95%. Reasons for not achieving DCC include cord snapping at birth, short cord, and severe placental abruption.
Overall, the implementation rates have improved and the change in practice has now been incorporated into routine practice. We will continue to review our data using NNAP on a monthly basis.
We also collected parents and staff feedback regarding the feasibility of providing DCC and delivery room cuddle using a simple template shown below.
Parent and Staff feedback forms:
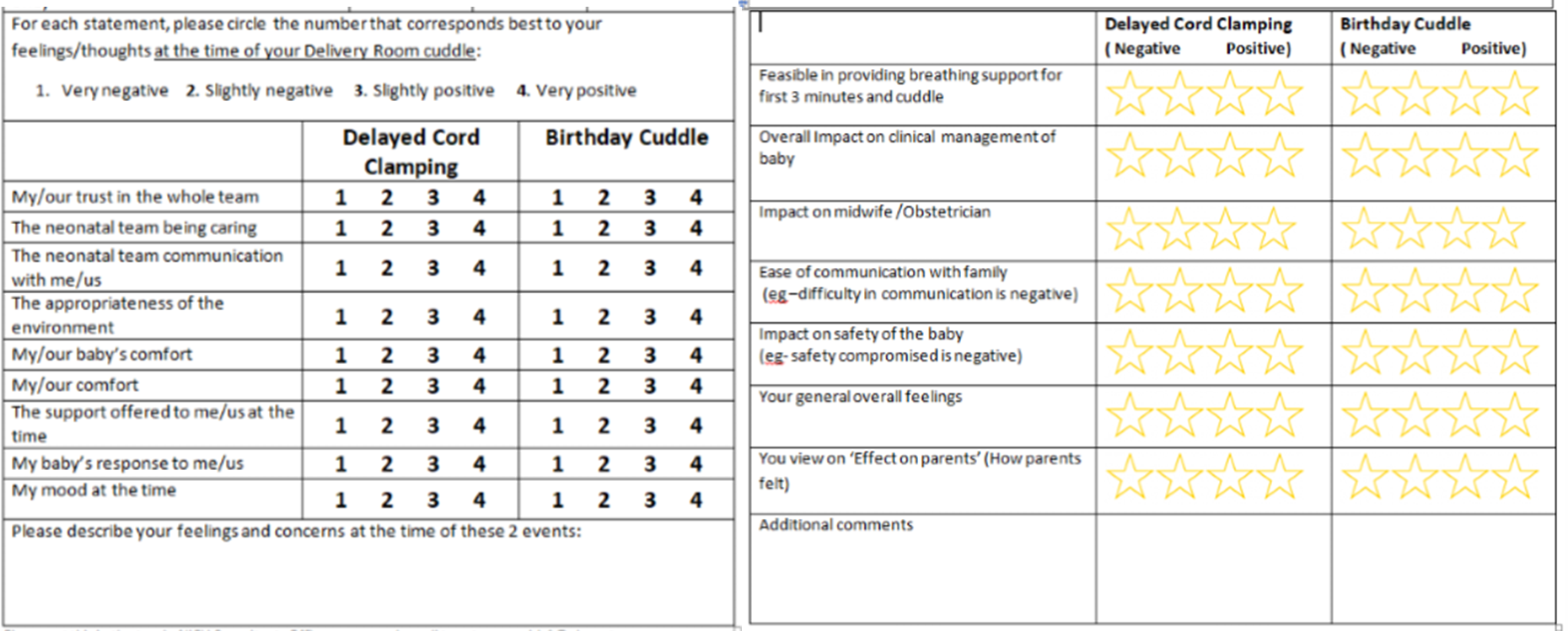
We received positive comments from parents and useful constructive feedback from staff that helped us to improve our practice. Some of the comments from parents were:
‘Didn’t really have concerns as it all happened very fast. I felt safe + well looked after. I trusted my baby was in the best care.’
‘I was nervous at first but felt so comforted by how contented my son was, he did not seem in pain or distress, the care was outstanding.’
Here are a few of the comments from staff feedback:
‘Parents gave the feedback on both elements, commenting they felt it was excellent to witness the stabilisation + the cuddle was lovely’
‘Worked well. Scrub nurse was very helpful for positioning LifeStart’
‘No room for me to reach baby to put on VT/do temp. VT wasn’t on and secured for a delayed period because I couldn’t reach.’
Additionally, we were able to achieve our secondary aims with >85% of babies being stabilised using our standard method – mobile HFNC; 89% with normothermia at admission; 84% receiving DRC or birthday cuddle and 82% with normal blood sugar at admission in the first year after implementation.
We aim to sustain the improvement through ongoing education on a 6-monthly basis at doctors’ induction, junior doctors to champion this project every 6 months, review NNAP data and present in meetings. Regular MDT simulations with obstetricians, midwifery and theatre staff have also been useful to sustain the momentum. Review of cases in mortality and morbidity meetings have also been helpful for educational purposes.
Challenges and learnings
As this QIP involved different team members from maternity, obstetric, neonatal nurses and doctors, anaesthetic team, and theatre staff, we were faced with a mammoth task of getting everyone on board. Therefore, it is really important to have an MDT set up right from the beginning with leads from all the areas to champion the change.
Often, there was more resistance in adapting this practice in caesarean sections due to the additional need for maintaining sterility and additional team members involved. Therefore, it is key to have theatre staff involved in this QIP.
Regular teaching and training sessions using simulation was very useful to ensure staff were familiar with the equipment, guidelines, and standard operating procedures.
Ongoing education using newsletters and sharing data/progress reports in quarterly governance meetings and quality and safety meetings were very useful to keep the momentum going.
Involving parents as a stakeholder is an essential key, and looking back at our QIP, we could have introduced this very easily at the beginning to motivate parents and midwives to be more involved.
Top tips for implementation
As we started this before the NNAP measure was introduced, we were leading on this in our network. Therefore, we have supported other Kent Surrey and Sussex (KSS) neonatal units by sharing our experience in network meetings and educational events.
We found it very useful to discuss the situation with other units who were already implementing DCC. Subsequently the lead consultant for this QIP provided 1 to 1 support to a number of doctors/midwives interested in implementing this in other units outside the network by showing them our practice and providing guidance as necessary.
We supported our KSS network by joining the working group and writing network guidelines to support every unit to implement DCC.
Authors: Dr Vennila Ponnusamy, Rebecca Piggott, Nadia Pridmore, Natasha Katsaros & Fiomena Leitao
Published as part of the NNAP Annual Report on 2020 data
Implementing Deferred Cord Clamping for Preterm Infants at a District General Hospital: A Multi-Phase Quality Improvement Project
York and Scarborough Teaching Hospitals NHS Foundation Trust
Background
DCC for greater than 60 seconds is a simple intervention which can be used to improve health outcomes for all babies, especially those born preterm. DCC is now recommended standard practice by the Resuscitation Council, British Association of Perinatal Medicine (BAPM), Royal College of Obstetrics and Gynaecology and World Health Organisation. There is increasing evidence to support the benefits of DCC including reduction in mortality, reduced risk of intraventricular haemorrhage and necrotising enterocolitis and improved cardiovascular stability. Since January 2020, data for the number of eligible preterm babies born <32 weeks receiving DCC has been collected as an NNAP measure. As DCC was not being performed for preterm babies born at our hospital, our unit specific data consistently highlighted this as an issue.
The aims of our project were reviewed and adjusted as the project progressed. Initially, during phase 2, our aim was that at least 80% of eligible babies born between 32+0 – 36+6 weeks gestation who were admitted to our level 2 neonatal unit should receive DCC for >60 seconds. We were aware that this would exclude some of the late preterm babies who were admitted directly to the postnatal ward but were happy to accept this for ease of data collection.
During phase 3, this aim has been extended to include all preterm babies <37 weeks gestation admitted to the neonatal unit, to be achieved by December 2021.
We initially completed a baseline case note audit to review how many babies between 32+0 and 36+6 received DCC between January and September 2020. A multidisciplinary team (MDT) including Paediatricians and Obstetricians developed a Standard Operating Procedure (SOP) document which was shared with the wider team prior to project implementation. Data was collected prospectively on a weekly basis using Badgernet and case notes to monitor progress. Results were shared monthly with all staff groups. Interventions were made using PDSA cycles to enable further improvement.
For this project to be successful, we were aware of the importance of involving key stakeholders with project planning and implementation. We worked closely with the lead obstetrician for the labour ward to ensure that the SOP was correct, and the roles allocated to team members were acceptable. The obstetrician was able to share plans with her consultant colleagues and address any concerns that were raised about this change in practice. She was also able to support this work further by sharing results and identifying solutions for any problems experienced.
Prior to progressing to phase 3(a), a MDT simulation exercise was conducted. This involved the preterm midwives, clinical skills midwife (educator), lead midwife for the labour ward, obstetricians and paediatricians. We recognised that staff involved with preterm deliveries need to be part of planning how DCC for this group of patients could be undertaken safely using existing equipment i.e. resuscitaires. Photographs were taken to add to the SOP so that the room and equipment setup was clear. The midwives have been able to share this information with their colleagues and therefore support DCC being performed routinely. Additionally, the lead obstetrician and paediatrician have both been responsible for ongoing training for their respective teams.
Measures
For phase 1, an initial snapshot audit was conducted over a one-week period in August 2020 on the postnatal ward to review the process of DCC in term infants. This identified that 56% (22 babies of which one was late preterm (36 weeks)) received DCC. The duration for DCC could not be identified in 6 cases; most of these cases were documented by medical staff. Learning from this audit was shared at local Clinical Governance (CG) meetings and reminders were sent to staff about the importance of clear documentation.
For phase 2, a baseline audit demonstrated that between January and August 2020, 31% (18/58) of eligible infants between 32+0 and 36+6 weeks gestation received DCC for >60 seconds. The findings were presented at Paediatric and Obstetric CG meetings to introduce the project and share plans for implementation. A standard operating procedure (SOP) was also developed and disseminated to the wider team for review prior starting the next phase.
Phase 2 commenced in October 2020 and data was shared monthly with the wider teams. These reminder emails enabled us to easily communicate any problems that were identified and next steps e.g. DCC timings not recorded therefore email reminder sent; when no improvement was noted, a photograph of how and where to document in the maternity and neonatal notes was also attached.
We recognised that DCC could also be impacting on the admission temperatures for our preterm infants, so we decided to collect additional data to monitor this.
Preparation for phase 3 started in April 2021. We sought advice from consultant neonatologists in our regional tertiary centres about their approach to DCC in early preterm infants and then conducted a MDT simulation to develop our local process. We decided to use our existing resuscitaire rather than a dedicated platform for DCC as this has been successfully done at a tertiary unit. Phase 3(a) was introduced in June 2021 after sharing an updated SOP in May for babies <32 weeks born on labour ward. Training has been provided for the paediatric and midwifery teams to ensure that staff are familiar with the process and their roles. Baseline data from October 2020 to May 2021 showed that an average of 41.7% of eligible infants received DCC >60 seconds.
We are currently planning how to progress on to phase 3(b).
Our improvement plan
Although DCC is routinely performed for term babies born at our hospital, this was not being done for any premature babies. We used a phased approach in collaboration with Obstetric and Midwifery colleagues to introduce this practice gradually, enabling staff to become familiar and confident with the process.
Phase 1: Audit practice of DCC for term infants
Phase 2: 32+0 – 36+6 weeks
Phase 3(a): <32 weeks born on labour ward
Phase 3(b): <32 weeks born in theatre (in progress)
- What changes did you make to result in an improvement?
- Please include details of barriers you faced and how these barriers were overcome.
Outcomes
There were a total of 173 babies admitted to our level 2 neonatal unit between 32+0 and 36+6 weeks gestation from January 2020 to July 2021. Of these, 156 were eligible for DCC and 17 were excluded from analysis due to contraindications for DCC (MCDA twins (14), placental abruption (1), cord prolapse (1) and significant resuscitation required (1)).
Prior to project implementation (pre-October 2020), an average of 54% of eligible babies received DCC which has improved to 78% post interventions. The graph below demonstrates this improvement:

There were a total of 22 babies admitted to our neonatal unit <32 weeks gestation from October 2020 to July 2021. Of these, 20 were eligible for DCC and 2 were excluded from analysis due to contraindications for DCC (MCDA twins).
Prior to project implementation (pre-June 2021), an average of 59% of eligible babies received DCC which has improved to 67% post interventions. The graph below shows this improvement:
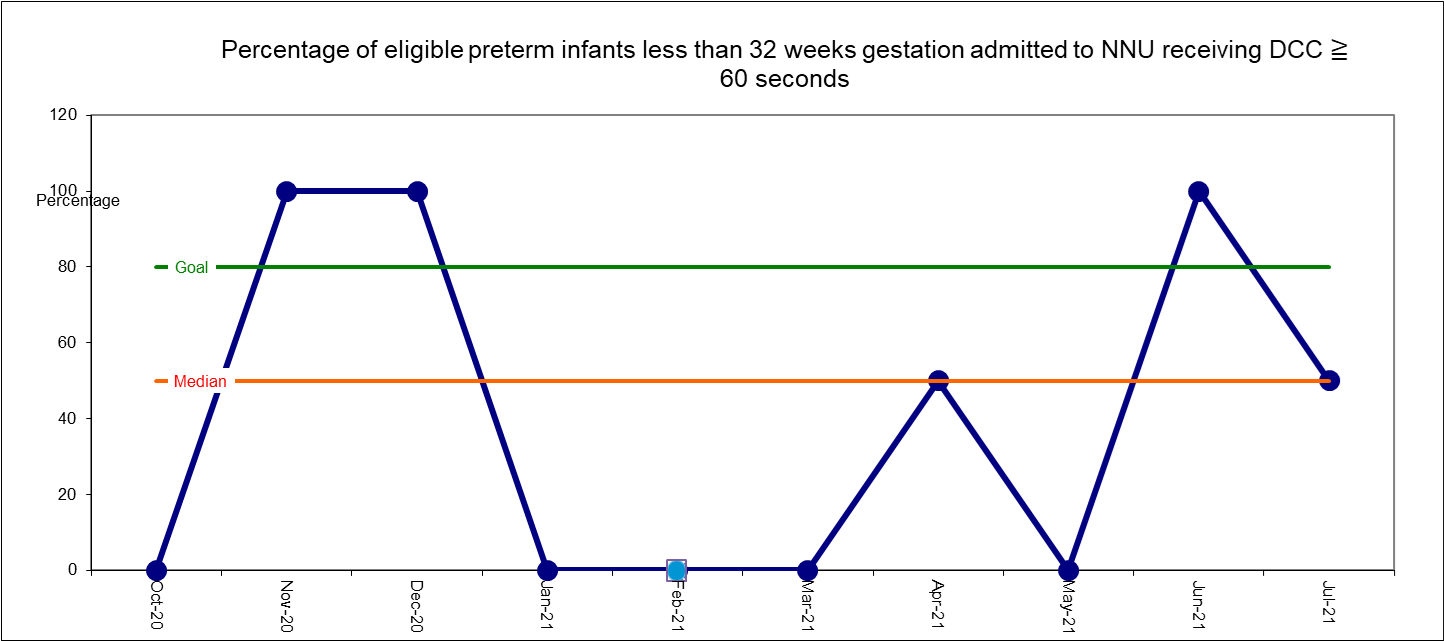
DCC is not being provided for any babies born <32 week gestations in theatre so we are expecting our results to improve further once this practice is introduced.
We are currently planning how to implement DCC for <32 week gestation infants who are born in theatre. Again, this will involve a MDT simulation exercise to identify our approach for this patient cohort. The SOP will be updated and shared with the team prior to progressing to this phase (3(b)). Whilst this project is continuing, we will continue to share results on a monthly basis to increase awareness and encourage this practice. The DCC figures are also shared as part of the ‘BAPM 7’ interventions for preterm babies at local CG and Maternity Safety Champions meetings.
Additionally, an introduction to DCC has recently been included within the paediatric induction programme for new junior doctors rotating to our department. We hope that as this becomes standard perinatal practice, our DCC figures will continue to improve. In the future, we plan to review those cases where eligible babies did not receive DCC so that we can identify and address any problems within our service.
Challenges and learnings
To date, this project has been progressing well with good engagement from all staff groups. The initial idea for how to undertake this project was based on what was being done at a tertiary neonatal unit within our network. The consultant responsible for this work was supportive and happy to share their plans and guidelines with us to adapt for local use. This provided a good foundation for us to build upon. We were also able to seek further advice from him as the project progressed which was particularly helpful.
In a busy working environment, finding time for regular data collection and development of resources was a particular challenge. The secret of our success was having a trainee who was able to dedicate time to this project (as he was spending time out of programme as a teaching fellow). It helps to have someone who can drive the project forward!
Additionally, it has certainly been helpful to have a multidisciplinary team of enthusiastic staff who have all been keen to make this project successful. We have shared the benefits of DCC frequently to try to get the wider team to understand why this practice is so important. Reminder emails, regular communication and on-going education has continued to raise awareness and ensure that staff are up to date with current plans. We hope that once phase 3(b) is introduced and DCC is being regularly performed at all eligible deliveries, our rates will continue to improve. We have been able to share our SOP within the network so that other units can also learn from our project.
Top tips for implementation
Following successful project progression at York Hospital, we are currently supporting the team at Scarborough Hospital (which is part of the same trust) to introduce the practice of DCC for preterm infants. Unfortunately, initial efforts in Scarborough were unsuccessful as the practice was introduced too quickly. We have found that using a multi-phased approach has allowed staff to become familiar with the process and increase their confidence with delivering DCC for more premature babies. We would encourage other units to adopt a similar approach if planning such a large-scale change in practice.
Additionally, working collaboratively with Obstetric and Midwifery colleagues has enabled this project to be successful and this change to gradually become embedded in practice. We hope that in the future, this will be a routine part of perinatal care within our trust. We also found that using existing equipment which the team were familiar with e.g. resuscitaire, meant that minimal additional costs and training needs have been associated with implementation.
Authors: Dr. Sundeep Sandhu (Consultant Paediatrician and Neonatal Lead, York Hospital) and Dr. Lawrence Wright (Clinical Teaching Fellow)
