Improving Rates of Optimal Cord Management in Preterm Infants Including Delivery of PEEP During Transition with an Intact Cord
This case study from Southmead Neonatal Unit in Bristol outlines how a multidisciplinary team worked together to achieve improved rates of optimal cord management. This quality improvement project was part of the PERIPrem (Perinatal Excellence to Reduce Injury in Premature Birth) initiative launched in the South West Neonatal Network.
Dr Heather White Neonatal Grid Trainee, Dr Fran Hoffmann, Neonatal Clinical Fellow, Dr Maria Tsakmakis Neonatal Consultant, Dr Faith Emery Neonatal Consultant, Dr Madhavi Parvathareddy Neonatal Consultant
Background
In April 2020 the quality improvement initiative PERIPrem (Perinatal Excellence to Reduce Injury in Premature Birth) was launched in the South West Neonatal Network. The aim was to implement a perinatal care bundle that would improve the outcomes of infants born at less than 34 weeks gestation. The bundle reflected the NHS Long Term Plan to reduce neonatal mortality and serious brain injury and is now part of the AHSN’s Maternity and Neonatal Safety Improvement Programme. The bundle consists of several perinatal interventions that demonstrate a significant impact on brain injury and mortality rates in preterm infants.
Over the following 6 months, the Neonatal and Obstetric Teams in Southmead Hospital focussed on the development and delivery of educational material to support and promote the launch of PERIPrem on 2nd November 2020. Education was delivered as focussed seminars as well as practical and simulation teaching on elements such as the delivery of thermal care and optimal cord management. In order to embed change of practice into the future team, educational sessions and supporting material were integrated into a new Induction Package for trainees. Prior to the launch of PERIPrem, large posters were displayed and emailed to each member of the MDT team to raise awareness of PERIPrem and to outline the achievement targets for each element. One of the main elements in the bundle was the facilitation of Optimal Cord Management (OCM).
Optimal cord management was recognised to be one of the more challenging elements of the bundle to implement into practice. This was due to the need for significant collaboration between several teams including the obstetric, neonatal, anaesthetic and theatre teams.
In October 2020 our rates of OCM were recorded as part of the regional QI project PERIPrem. We were successfully delivering OCM for 60 seconds or more in infants <34 weeks in 33% of cases. At this time there was no formal guidance available in the Trust on how to achieve the effective delivery of OCM in the preterm population and OCM delivery with PEEP support was not performed routinely.
It was imperative that the Neonatal, Obstetric, Anaesthetic and Theatre teams met to discuss how to achieve OCM and to bring to the forefront any perceived barriers to its success. Face to face meetings were impossible due to the restrictions placed upon us in the COVID-19 pandemic and so virtual meetings on MS Teams were instigated.
The main perceived barriers identified during these discussions were:
- The current ineffectual communication of the ‘intent’ to deliver OCM to a baby between the obstetric and neonatal teams. The obstetric team expressed that they often felt uncertain as to whether this was something the neonatal team would like in a preterm baby as they felt the neonatal team would like the baby brought to the resuscitaire as quickly as possible.
- A lack of clarity as to who would take responsibility for assessing the infant and deciding when to clamp and cut the cord (providing there was no maternal complication when the obstetricians would automatically cut the cord to stabilise the mother). The perception of the obstetric team was that it was their decision as to when to clamp the cord and they felt that they lacked the expertise to assess infants at the extremes of viability
- The absence of a ratified guideline on how to facilitate delayed cord clamping whilst delivering thermal care in different clinical settings i.e., theatre and delivery suite, meant that there was significant variation between individuals’ actions and expectations which could lead to confusion
- Uncertainty from the neonatal team as to whether we could provide PEEP during optimal cord management due to concerns being raised by the anaesthetic team regarding the infection risk of using clean rather than sterile extended PEEP circuits
The discussions that took place were very interesting and highlighted that the perceived barriers by all teams were predominantly based around communication and standardisation of practice. The involvement of multiple teams with representation from each level within that team was the key to the success of these meetings. The voice of the theatre staff, midwives and junior medical team who attend the majority of deliveries was an integral part of the process.
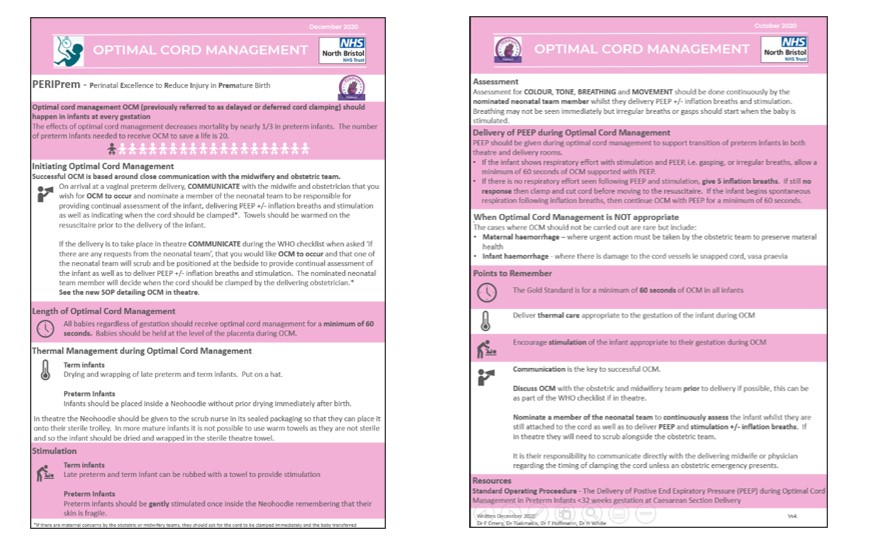
An educational leaflet was created and circulated to all members of the MDT in which the evidence base for delivery of OCM, the expectations of our Trust for its delivery and guidance on how to achieve this in the preterm population was documented.
Figure 1. Samples of educational material regarding Optimal Cord Management developed in North Bristol NHS Trust
Measures
We performed two PDSA cycles focussed on the delivery of OCM in the 6 months following the introduction of the PERIPrem bundle. Data was collected as part of the PERIPrem project and analysed on a monthly basis. The raw data was interrogated, and each infant’s case was individually reviewed to look for reasons that OCM was not achieved.
Reasons for OCM not being performed varied from the unexpected snapping of the umbilical cord or rapid separation of the placenta, to infants being identified as being in poor condition following delivery resulting in precipitous clamping and cutting of the cord. Occasionally no reason was recorded in the medical notes to explain the absence of OCM.
Our improvement plan
New BAPM guidance on OCM was released in November 2020 and in discussion with the MDT, it was decided that we would introduce the delivery of PEEP during OCM to infants <32 weeks gestation.
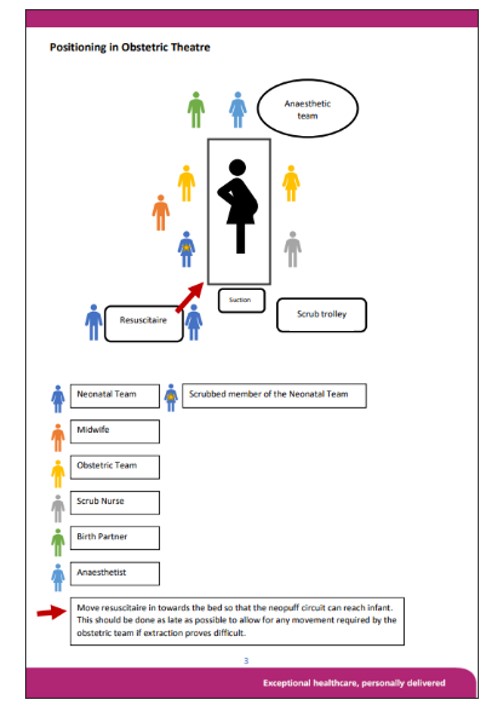
Rather than host a formal meeting to facilitate a discussion, an MDT ‘walk through’ in the theatre setting was suggested to enable all teams to visualise the process and identify potential barriers. A C-Section delivery was simulated from start to finish and the optimal positioning of team members around the patient, the critical points of important communication and the roles of team leaders were decided.
The MDT walk through led to the following points being agreed between the teams;
- The expectation in all preterm deliveries is that OCM should be delivered unless there was haemorrhage that would compromise the mother and/or infant.
- A lead neonatal team member will be nominated at the start of all deliveries and will be responsible for assessing the infant whilst attached to the cord. In theatre, this person will be scrubbed and stand at the side of the mother behind the obstetrician. They will decide when the cord should be clamped and cut. The obstetric team will be responsible for recommending immediate cord clamping if required for maternal health.
- The intent to deliver OCM in theatre during a sterile C-Section should be declared in the WHO checklist prior to commencement of the C-section delivery.
- The use of clean, long PEEP circuits (2m in length) can be used to offer PEEP whilst the cord is intact in the sterile environment
- Neohoodies should be used in all preterm infants to optimise thermal care whilst attached to the cord. In theatre the Neohoodie should be given to the scrub nurse to place on the sterile trolley with the instruments
- The decision was taken not to use a Lifestart Trolley to facilitate OCM due to the space limitations in the Obstetric theatres. As an alternative, the positioning of the team around the patient was optimised and the roles assigned to different members of the team were confirmed and standardised.
- The open Neohoodie would be placed on the mother’s legs by the scrub nurse to enable the obstetrician delivering the baby to place the infant inside.
- The Neonatal lead would assist the Obstetrician placing the infant in the Neohoodie to allow them to focus on delivery of care to the Mother. The Neonatal lead would then support the infant whilst assessing them
- A clean, extended 2m PEEP circuit and facemask would be passed to the neonatal lead by the neonatal support team at the resuscitaire to enable them to deliver PEEP to the infant
A standard operating procedure for the delivery of OCM with PEEP in infants <32 weeks was written and agreed by all teams in December 2020 and was introduced in January 2021.
Figure 2. The positioning of team members as dictated by the SOP for Delivery of OCM with PEEP in preterm infants in North Bristol NHS Trust
Outcomes
All data displayed in this section is local data for North Bristol NHS Trust, collected as part of the regional QI project, PERIPRem.
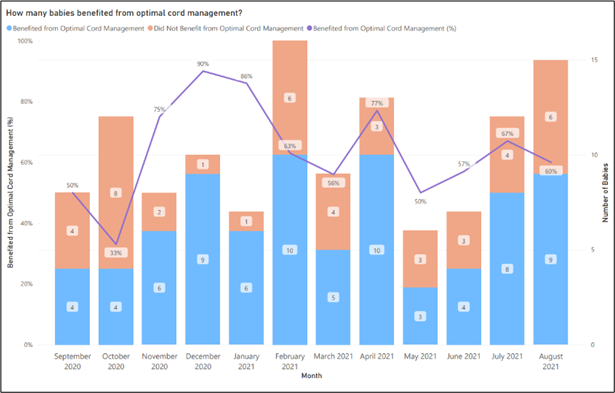
The first PDSA cycle in November 2020 showed that the delivery of OCM for 60 seconds or more in eligible preterm infants improved from a baseline of 33% to 75%.

Further teaching and OCM simulations were delivered at Tier 1 and 2 teaching sessions throughout December and at the end of 2020 the successful delivery of OCM had surpassed the target of 85%, reaching 90%.

In January, the second PDSA cycle resulted in the introduction of PEEP during OCM. Simulation sessions with the MDT and circulation of a SOP supported this development. Despite this change in practice, the rates of OCM remained above the set target.
NNAP data for 2020 showed that there were 80 preterm infants eligible for OCM and 59.5% achieved 60 seconds of OCM compared to the national average of 28.9%.
The statistical process control chart (SPC) derived from PERIPrem data clearly shows the positive response to our educational programme and the introduction of guidelines and SOP from October 2020 to January 2021. The subsequent reduction in achieved rates of OCM in February and March was attributed to the influx of new trainees within the obstetric and neonatal teams. The next 6 months saw the rates of successful OCM fluctuate but settle at approximately double the initial figure achieved.
Figure 3. SPC Chart for OCM created by PERIPrem.
Reference. The PERIPrem Bundle: Perinatal Excellence in Reducing Injury in Premature birth – Dr K Luyt, Strategic Clinical Lead Karen.Luyt@bristol.ac.uk, Ellie Wetz, Programme Manager, West of England AHSN Ellie.wetz@weahsn
Quarter 4 NNAP data in 2021 demonstrated a sustained level of delivery of OCM above the national average (43%) at 57.7%.
Challenges
The challenge moving forward is embedding the changes we have made into clinical practice. Bringing the importance of OCM to the forefront in our Trust definitively changed the attitude of all teams attending a preterm delivery in Southmead Hospital. The ‘decision’ to deliver OCM is no longer a decision, it is the standard of care expected for the preterm infant. It is facilitated unless there is a significant contraindication to mother or baby. This change in mindset has been supported by the educational programme which provided staff with the evidence base to support their actions.
The relationship between the obstetric and neonatal teams has also evolved. Communication when attending deliveries is clearer and more concise with roles within teams being more clearly defined and recognised. Staff have developed confidence in delivering OCM and are aware of the expectations of their colleagues. This has led to a synergy in the Womens’ and Childrens’ Department that did not exist so clearly before.
With such a clear benefit to preterm infants, it is important that we strive to improve our delivery of OCM beyond its current levels. We have shown that education in the form of simulation and seminar-based teaching works well but with the high change over rates of staff in our field it is imperative that these teaching sessions are delivered regularly and especially in the induction sessions for new starters.
We recognise the importance of staff being informed of the monthly rates of OCM as it enables them take pride in the good outcomes achieved. It also offers opportunity for reflection in less successful months and generates discussion and innovation for future developments. During the first 6 months of implementation of PERIPrem a monthly newsletter was sent out to all staff displaying the rates of each element achieved and offering pointers for development of practice. These were received positively by the teams.
Lessons learnt
The main challenges encountered in this project were based around communication. Firstly, the implementation phase of the project was during the height of the COVID-19 pandemic when teams were stretched and face to face communication was difficult. But learning to adapt to a changing situation is what actually defined this project. The rapid introduction of virtual meetings meant that we were able to bring together many more individuals than we would have achieved face to face. This meant that the representation of roles within the different teams was much wider resulting in discussions being more inclusive and pragmatic.
Another challenge that required adaptation in our practice was the spatial limitations in the Obstetric theatre which made use of the LifeStart Trolley impractical. It was only through establishment of close communication between teams and standardisation of the process of delivering OCM that has enabled us to maintain thermal care and deliver OCM with PEEP to even the most preterm infants. When infants are at the extremes of viability the short length of the umbilical cord requires extremely close, delicate and intricate care from an obstetrician and neonatologist who can work and communicate in complete synergy.
Acknowledgements
We would like to thank the PERIPrem team for the data displayed as well as their support in the implementation of the PERIPrem bundle including OCM in our Trust.
