Prevention of Cerebral Palsy in Preterm Labour (PReCePT)
A scalable quality improvement initiative co-designed, with parents, obstetric, midwifery and neonatal clinical teams in West England to increase the uptake of Magnesium Sulphate given intrapartum during preterm labour.
Background
Being born preterm is the leading cause of Cerebral Palsy (CP), with lifelong impact on children and families. Magnesium Sulphate (MgSO4) given intrapartum during preterm labour reduces the relative risk of CP in very preterm infants by 30% 1. The number needed to treat (below 30 weeks gestation) to prevent one case of CP is 37 2, and yet UK use was inconsistent 3, leading to preventable health inequalities.
In West England we co-designed, with parents, obstetric, midwifery and neonatal clinical teams, a scalable Quality Improvement (QI) initiative called PReCePT (Prevention of Cerebral Palsy in Preterm Labour), which was piloted as PReCePT1 in five maternity units from 2015. The uptake of MgSO4 increased from 21% to 88% within 6 months 4. PReCePT1 influenced the UK national preterm labour guideline, which recommends intrapartum MgSO4 in preterm labour, < 30 weeks gestation 5.
PReCePT1 achieved:
a) scalable QI intervention ready for national adoption/spread
b) development of the national metric for MgSO4 uptake, in partnership with the National Neonatal Audit Programme (NNAP).
In 2018 the Health Foundation funded us to scale-up and research how best to support teams to adopt PReCePT 6. The national implementation of PReCePT was commissioned by NHS England to be delivered by the Academic Health Science Network (AHSN) across England 7.
Measures
The primary measure is percentage uptake of MgSO4 per unit as reported by NNAP. The size of the national adoption problem became evident in the 2017 NNAP report. Only 44% of preterm babies received the benefit of MgSO4 neuroprotection, with large variability (26-71%) between Operational Delivery Networks (ODNs).
Our improvement plan
The aim:
For every maternity unit to adopt the NICE NG25 guidance and achieve 85% uptake of administration of MgSO4 to eligible mothers in preterm labour in England by April 2020.
A novel network QI delivery model:
- delivery by 15 AHSNs, aligned to Neonatal ODNs, in all 152 maternity/neonatal units
- regional QI and clinical leads, working with unit-level midwife champions (clinical time funded)
- PReCePT obstetric and neonatal lead in each unit, enabling a perinatal team approach
- standardised QI resources (toolkit, implementation guide, training presentations and promotional collateral) 7
- nested randomised control research trial, in 40 maternity units, designed to assess the effectiveness of two different QI implementation methods 8
Outcomes
Mean average MgSO4 uptake achieved in England in 2019 was 84.9%.
Variability between English ODNs was substantially reduced (range in 2016: 26-71% vs. range in 2019: 77.5-93.7%). The likely impact will be a substantial ongoing reduction of avoidable cerebral palsy. PReCePT enabled a national perinatal QI network and will provide best practice evidence for national scaling up of perinatal QI initiatives.
Supportive quotes from service users and perinatal teams:

Case example from Watford General Hospital:
Woodland Neonatal Unit at Watford General Hospital, West Hertfordshire NHS Trust is Local Neonatal Unit within East of England Neonatal Network and cares for around 1200 neonates each year. Our unit has actively engaged with National Neonatal Audit Programme (NNAP) since its inception in 2007. Research has shown that magnesium sulphate (MgSO4), given antenatally in threatened preterm labour, is neuroprotective and reduces cerebral palsy. In preterm infants born less than 30 weeks gestation use of antenatal MgSO4 is benchmarked as an NNAP audit measure.
Watford General Hospital was an outlier for this audit measure in the 2017 NNAP report (2016 data). In this case study, we demonstrate how we have used NNAP antenatal MgSO4 data benchmarks to guide our quality improvement project and improved MgSO4 uptake in eligible preterm deliveries. Moreover, we have raised team awareness, built intrinsic team capability, encouraged parent involvement and offered an informed treatment choice.
Our improvement plan:
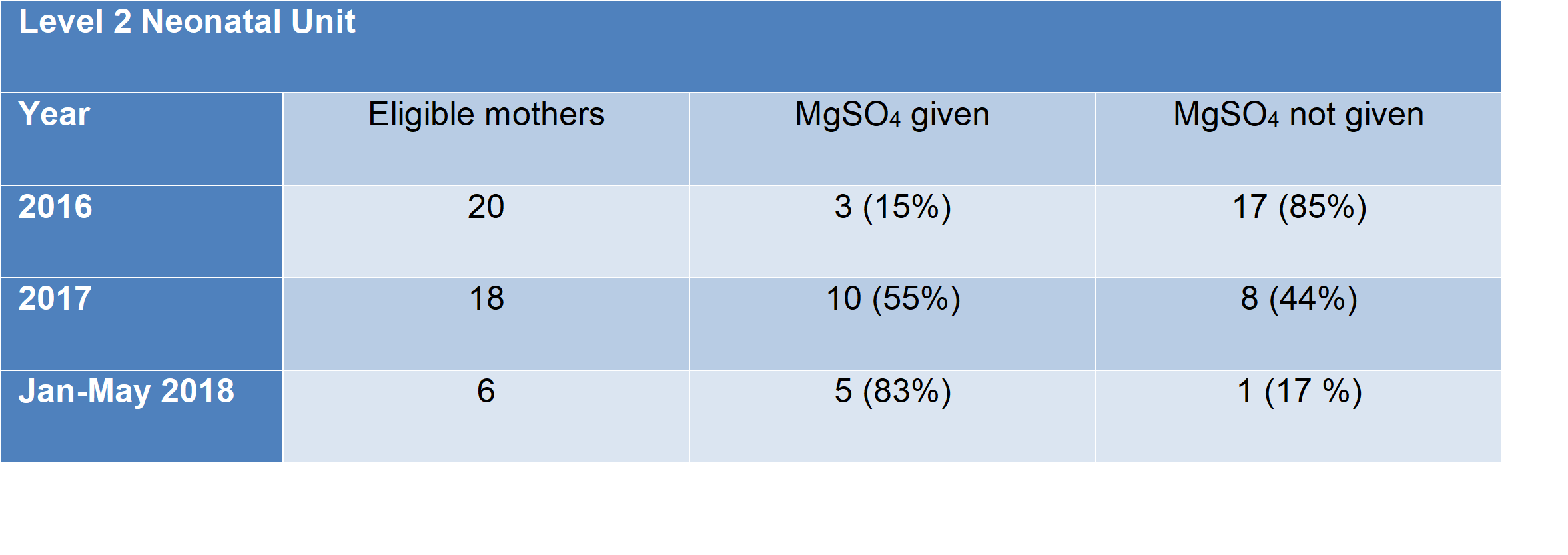
Our improvement journey started in 2016, when we became aware that our neonatal service was an outlier for antenatal magnesium sulphate (MgSO4) administration with an uptake 15%, which was far below the national average (43%).
Strategy for change:
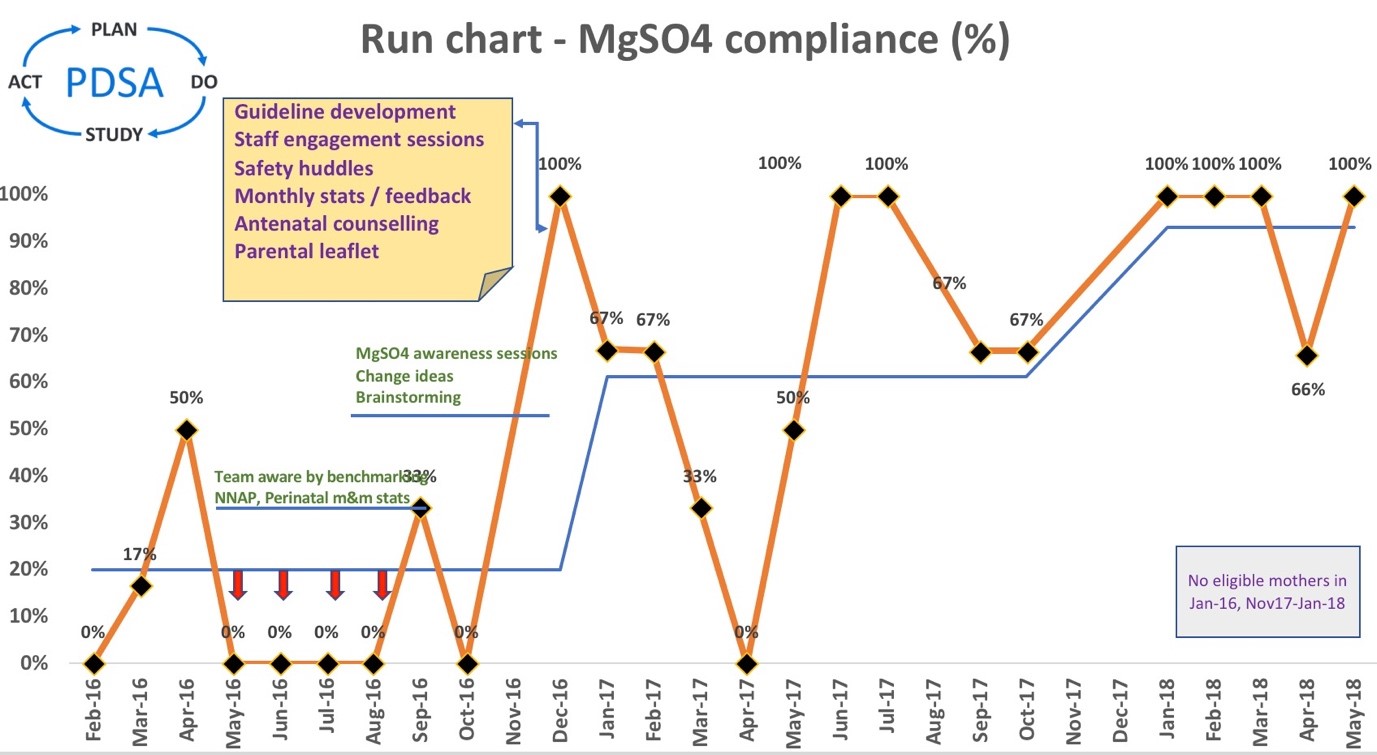
Using the Institute of Healthcare Improvement (IHI) model we aimed to increase the uptake of MgSO4 in eligible preterm deliveries. Improvement measure was defined as an increase in the uptake of MgSO4 from 15% in 2016 to 40%, hence reaching the then national average. Primary, secondary drivers were identified which informed change ideas. These changes were tested in iterative plan, do, study, act (PDSA) cycles.
What we did:
Development of a driver diagram allowed us to conceptualize the issue and determine the pathway to achieve our goal. Using this tool with its excellent visual display of change ideas, we could have brain storming sessions and engagement between the relevant stakeholders such as midwives, obstetricians and neonatal staff and discuss potential solutions:

We created a run chart, to display compliance data in % (y axis) over time (x axis). It’s a simple and effective QI tool we used to formulate the aim and engage the stakeholders by depicting the MgSO4 compliance monthly. In addition, the run chart was guiding the improvement team to determine if the changes we were making are leading to improvement:
Change package:
We have increased awareness amongst the neonatal, obstetric and midwifery teams by presenting run chart data (Figure 2) in monthly Perinatal Mortality and Morbidity meetings. We commenced frequent bitesize MgSO4 awareness and engagement sessions with all the stakeholders. A new and simple guideline for MgSO4 administration was developed and implemented and we encouraged 1:1 midwifery care in labour. Safety “huddles”, twice daily board rounds, were introduced to identify all eligible women. Additionally, we involved the service users, by providing them with a parental information leaflet with the antenatal counselling pack and MgSO4 information were included in the antenatal counselling conversations and golden hour care checklist.
Challenges:
Main challenge was to change staff’s ethos and perceptions, bring down the “barriers” and move away from the culture “this is how we do it for years and it works for our patients”. We achieved this by enhancing communication and knowledge sharing through safety huddles, identifying clinical champions to support the team, presentations in joint multidisciplinary team forums and empowering ward level leadership. Encouraging parent involvement raised further awareness of this important neuroprotective treatment.
Outcomes:
According to NNAP 2016 report only 15% of eligible women received antenatal MgSO4 at Watford General Hospital, compared to a national average of 43%. The table below shows steady improvement from 2016 to 2018 with the implementation of change ideas. The 2017 data show that we met and surpassed our improvement target achieving a compliance of 55%, well above the national average. The 2018 NNAP data shows further improvement and a sustainable change. This sustainable improvement has a direct impact on the long-term neurodevelopmental outcomes and by extension to the quality of life of preterm infants born at less than 30 weeks of gestation:
Top tips for implementation:
- Identify an appropriate maternity-neonatal forum to share NNAP MgSO4 data
- Identify and engage stakeholders and frontline champions within maternity and neonates
- Use live NNAP dashboard on Badgernet to generate live run charts
- Partnering with parents for improvement
Acknowledgements:
Justine Chung, Matron, Delivery suite
Bhavani Sivakumar, BadgerNet data analyst
Authors:
Dr Sankara Narayanan (Consultant Neonatologist & NNAP lead), Dr Anastasia Katana (Locum Consultant Neonatologist), Ms Nanda Shetty (Consultant Obstetrician), Ms Marcellina Coker (Consultant Obstetrician)
Neonatal & Obstetrics Department, Watford General Hospital, West Hertfordshire NHS Trust

PReCePT Challenges and learnings
Lessons learnt to foster success:
- Place babies and families at the heart of the programme – parent advisers have strongly advised that MgSO4 be offered to all eligible mothers to help improve the life chances of preterm babies (see video clips below):
- Funded support/time for front-line clinicians to deliver the project key to successful delivery
- Fostering a perinatal team, joining together obstetric, midwifery and neonatal clinicians – developing perinatal clinical leadership in every unit (see video clip below):
- National strategic alignment to the Maternity and Neonatal Safety Improvement Programme and ODNs
- Positive use of social media to engage a truly national PReCePT community – see @PReCePT_MgSO4 and @PReCePT_Study on Twitter
Challenges:
- Designing a project that was responsive to differences in unit level culture and microsystems
- High number of stakeholders to engage/coordinate with, challenged by regional variation
- Access to real-time data to support the monitoring of MgSO4 uptake
Top tips for implementation
- Engage and empower perinatal clinicians to lead at local and regional level
- Provide the QI skills, evidence and support to effect change
- Create a social media community of practice and communication plan
- Development a metric for national measurement of MgSO4 uptake, utilising routine data
- Influence national policy; MgSO4 neuroprotection has become routine practice by inclusion in the NHS Long-Term plan 9, “Saving Babies’ Lives Care Bundle” 10 and NICE guidance 5, enabling sustainability of uptake.
Acknowledgements
- West of England Academic Health Science Network (WEAHSN)
- National Academic Health Science Network
- University Hospitals Bristol and Weston NHS Foundation Trust
- The Health Foundation
- National Institute for Health Research Applied Health Collaboration West (NIHR ARC West)
Authors: Karen Luyt (PReCePT Programme Clinical Lead and PReCEPT Study Chief Investigator), Ellie Wetz (Programme Manager), Pippa Craggs (PReCePT2 Project Manager)
Organisations: West of England AHSN and University Hospitals Bristol & Weston NHS Foundation Trust
First published in the NNAP Annual Report 2020
PERIPrem – Perinatal Excellence to Reduce Injury in Premature Birth
Background
Prematurity is the single biggest cause of neonatal and infant mortality in England. NNAP (2016-19) reported 1,400 deaths before 32 weeks gestation with significant regional variation, not explained by differences in case mix. National analysis (2019) demonstrates scant reduction in newborn brain injury rates over the previous 4 years. The NHS currently falls short of the target of a 50% reduction by 2025. The 11 interventions within PERIPrem could achieve at least a 50% reduction in mortality and severe brain injury, if implemented as a bundle.
Optimisation of the preterm infant is complex; eligibility for treatments is dependent on gestation, birth weight and local policies. Preterm infants experience variability in care dependent on the place of birth, and there remains an implementation gap for several evidence-based treatments (notably optimal cord management and early breast milk). The geography of the South West further complicates delivery of optimal preterm care, compounded by demographic variables in population served such as the differing demands of rural and urban centres.
PERIPrem sought to establish a committed, multi-organisational collaborative that continues to drive perinatal improvement using a common language and streamlining processes. In addition to saving the lives of the most vulnerable babies, PERIPrem aims to improve the chances of disability free lives and is nurturing high-functioning perinatal teams with QI skills.
Perinatal teams in all 12 Trusts were asked to collect data to measure for improvement using a bespoke PERIPrem QI data collection tool. This tool allowed real-time assessment of optimal care, as well as aggregate data at Trust, sub/regional level. This data provided teams with the opportunity to celebrate successes and identify further opportunities for continuous improvement.
This data was also supported by a quarterly dashboard commissioned by the South West Neonatal Network that extracted anonymously aggregated data directly from the neonatal electronic patient record. This served as an effective quality check for NNAP nationally reported data sets. PERIPrem is being independently evaluated by the South West AHSN with publication planned for early 2022 with measures around improving perinatal team working and collaboration.
Recognising bundle size, geography and reliance on ownership for success, PERIPrem invested in bringing together organisations across two regions. Led by the West of England and South West AHSNs, it was designed to maximise collaboration of perinatal teams including; 12 NHS Trusts, the South West Neonatal Network, NHS England South West Maternity Team, parent partners and clinical experts resulting in the UKs largest perinatal QI clinical collaborative.
PERIPrem was driven by perinatal clinicians to ensure the bundle resulted in intuitive, evidence-based, sustainable improvements designed to fit the culture of the units.
PERIPrem collaborated with Health Innovation Network and Hologic to learn from work on the QUIPP app, to rapidly standardise the use of Quantitative Fetal Fibronectin Testing across the region and supported the development of the BAPM Optimisation Toolkits. Our collaborative approach involved keeping key LMNS partners involved in the progress of the project. An outline of the project can also be found online on the South West AHSN website here.
Measures
PERIPrem was modelled on the highly successful programme PReCePT – originally piloted in the West of England and then rolled out nationally via the network of AHSNs, with the aim to increase uptake of magnesium sulphate during preterm labour. This model empowered clinical leaders (Neonatal nurse & Midwife, supported by a Neonatal Consultant and Obstetric consultant in each of the 12 units) at unit level to use QI science and methodologies to improve mother/baby exposure to evidence-based clinical interventions. PERIPrem resources were developed to support unit level clinical leads on their QI journey, supported by regular coaching session from AHSN QI specialists and clinical experts.
PERIPrem was planned to be delivered face-to-face using the principles of an IHI Breakthrough Series Collaborative. Unfortunately, it also timed with the advent of the global COVID-19 pandemic. In order to deliver PERIPrem during this challenging time, our strategy pivoted – all engagement was via online platforms either as direct 1:1’s or shared learning events. This model had some positive unintended consequences: unit level clinicians were more accessible and could build in PERIPrem sessions into their working day; sessions could be recorded for later play back; teams from different units could meet and collaborate; regular subject matter topic experts could be seconded to the project to support the delivery of specific perinatal interventions.
All 12 PERIPrem teams were given access to Life QI to manage their QI projects for specific interventions. This platform allowed them to record their PDSA cycles and plot their process measures for continues analysis and improvement. The project team were able to review and share the programme progress as a whole and add resources centrally for all to make use of.
For one specific bundle element, optimal cord management, unit level teams were coached regularly to identify and overcome their own barriers, often sharing experiences with other teams around common barriers of delivering thermal care and respiratory support in a sterile way. Teams also identified their own enablers, and rapidly spread these across the entire region for collaborative improvement. Several teams filmed their techniques for OCM to support and educate other PERIPrem teams regionally.
Our improvement plan
Launched in April 2020, PERIPrem is a perinatal care bundle to improve the outcomes for premature babies across 12 maternity and neonatal units in the West and South West regions. The bundle consists of 11 perinatal interventions that will demonstrate a significant impact on brain injury and mortality rates amongst babies born prematurely. PERIPrem seeks to optimise preterm care through improving perinatal working using QI methodology.
To address the problem of reducing system variation and optimising care, PERIPrem recognised the need to bring together all partners involved at regional level. This included designing a quality improvement data tool, establishing a perinatal clinical collaborative, and putting parent partners at the centre.
Whilst the majority of the 11 bundle elements were current practice to some degree in most units, the introduction of PERIPrem resulted in all 12 units delivering a standardised care bundle dependent on gestation and weight.
Outcomes
PERIPrem highlights how multidisciplinary teams of all specialties can improve functionality and increase psychological safety to optimise patient care and improve outcomes, working in alignment with unit culture and processes.
A valuable outcome facilitated by PERIPrem is a shared language of perinatal improvement, through the regional roll out of a parent passport and a clinical passport to streamline and standardise care given at all hospitals across the network, improving patient experience particularly when there is a need for transfer.
PERIPrem is highly valued by the unit teams. The ability to connect with formerly unknown peers through PERIPrem, working on the same improvement provides opportunities for continued innovation across an even wider geographical area:
“The enthusiasm of the PERIPrem Team is contagious. The support they have provided us to implement changes in practice that are essentially life changing to our premature babies has been invaluable. Proud to be part of the PERIPrem family” – Pauline Hewitt, Midwife, Gloucestershire Royal Hospitals
PERIPrem placed parent partners at the heart of the programme to ensure co-production. Parent partners are members of the PERIPrem steering group alongside lead clinicians and representatives from maternity and neonatal systems, contributing to strategic development. Our parent partners are hands on with design and development of parent facing resources and have led “share and learn” sessions for perinatal staff and provided a link to wider patient networks;
“Being a parent rep on the PERIPrem steering group has been one of the most empowering journeys I have taken as a Mum of a pre-term baby. Seeing my ideas incorporated into the design and roll out of the PERIPrem bundle has been incredibly rewarding. It’s knowing that I have made a personal difference” – Leanna Wakely, PERIPrem Patient Partner
The collaborative development of the Optimisation Tool allows contemporaneous data to be shared at unit and regional level, strengthening the collaborative approach to improvement. The regional dashboard facilitates rapid review of cases, including mothers transferred between hospitals, to compare, learn and make pathway improvements. As an outcome, the tool has emerged as a key factor in facilitating collaborative working for improvement. All users are encouraged to suggest modifications to the tool, and newer versions then issued for testing. This tool is the result of PERIPrem collaboration and provides a solution to shared data.
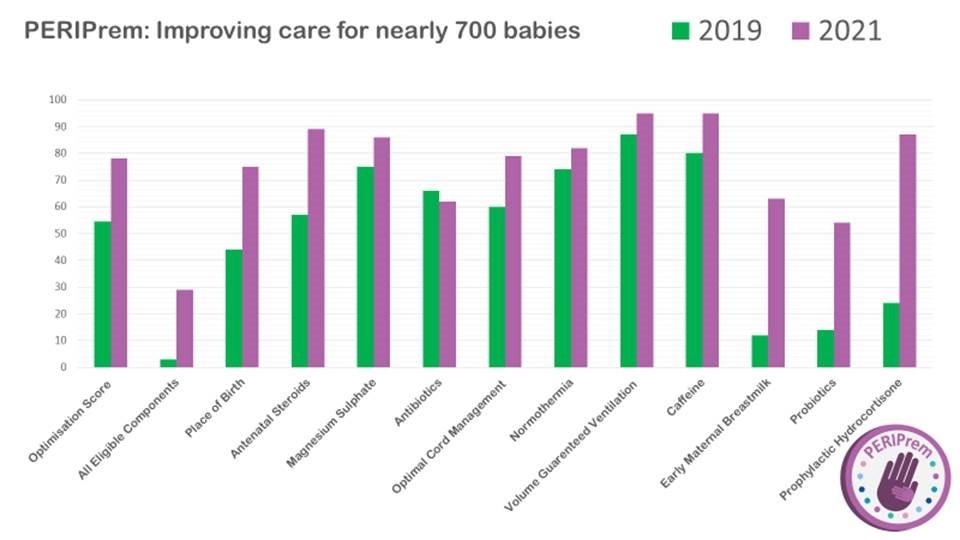
The chart below provides an overview of improvements made using the PERIPrem QI data collection tool:
Challenges and learnings
PERIPrem empowers perinatal teams to take ownership of implementation and work together as a region or clusters of units to share learning. To facilitate this in the restrictions placed by the pandemic, we supported teams and member organisations (including parents) to host share and learn sessions on specific elements, regularly providing recorded opportunities for clinicians and the wider perinatal community to collaborate. This increased access to experts across the region and maximised support for teams when capacity was under the most pressure.
Reaching the point of full participation of all 12 units required targeted, persistent coaching in the face of competing demands including navigating the impact of COVID 19. In order to achieve full engagement of all trusts, senior leadership figures were recruited to promote participation alongside data sharing within LMNS patient safety settings.
Responding with agility to the restrictions of the pandemic has resulted in a wide range of webinars, share and learn sessions and other resources moving into the virtual space, these are available on the PERIPrem website for other regions and systems to learn from alongside QI/implementation tools, learning materials, coaching tools, run chart templates and PERIPrem clinician and baby passports.
We hosted some virtual open QI clinics for our PERIPrem leads as an opportunity to ask questions from a QI expert, their coaches and to share learning with each other. Our network in person events were cancelled due to the pandemic and we felt that teams has missed out an opportunity to get to know each other. However, these weren’t as well attended as we’d hoped due to clinical pressures; there are only so many virtual events you can fit into your lives!
Due to the national heightened sense of pandemic stress we focussed on celebrating success with the teams and raising awareness across the system if someone had had a win, no matter how small, encouraging pictures to be shared, WhatsApp groups to be set up and attempts to foster a sense of supportive camaraderie regardless of the fact that no one had actually met each other in person.
During some initial coaching calls it was noted that some teams faced some internal politics when reviewing and agreeing priority project steps. We decided to fund 2 share and learn opportunities with a culture expert who was very familiar with the South West maternal and neonatal SIP teams to provide both some broad and bespoke advice, as required. These sessions were well attended and evaluation feedback positive. These teams reported and increased sense of teamwork in their qualitative interviews
Top tips for implementation
PERIPrem has resulted in a innovative methodology that can be applied to other areas of multidisciplinary QI. We have refined an extensive range of tools and approaches to working across a wide geography that are accessible for free.
As a large regional pilot, PERIPrem offers a replicable opportunity to be spread to other geographical areas & clinical specialities, in particular, we have invested in developing perinatal team culture, recognising that to improve safety, and multi-disciplinary team working must be optimised.
The South West geography made navigating a regional QI programme challenging but allows testing of spread and adoption across twelve units of differing level of care, population demographics served and location. This includes smaller local neonatal units and three tertiary regional centres, two of which are in Bristol, an urbanised area, compared to Plymouth tertiary centre, with a different population.
Our collaborative approach with the South West ODN and various industry partners has meant that the outputs from PERIPrem have spread organically through a variety of networks. Where asked the PERIPrem project team have always supplied information and presented the project work for shared learning and opportunities to spread. Our aim has always been to make the replication of this project and it’s learnings available to all without cost for an increase in speed and adoption of outputs, maximising benefits to premature babies and their families.
One other region (Yorkshire & Humber) have gone live with the PERIPrem passport, and further interest has been shown by other networks in the UK, in addition to some international interest for PERIPrem implementation from Sri Lanka.
The benefits of the PERIPrem patient passport have been of particular interest to people who have benefitted from their usage during their premature birth experience. We have captured some of these patient experiences on film clips which are freely available on the PERIPrem website for all to access and use. As the use of these passports is embedded and sustained in our region, where they “cross-over” to out of region transfer opportunities we expect additional interest and questions on the project from both clinicians and families respectively.
The PERIPrem website has over 8000 views since August 2020 with the @peri_prem twitter handle receiving 144,000 impressions, 5700 profile visits, 400 new twitter followers and over 700 features with #periprem. As the PERIPrem evaluation is published and circulated we anticipate further increases in these communication statistics with growth around resource downloads, twitter followers and project replication.
Authors: Sarah Bates, Karen Luyt, Ellie Wetz, Sally Hedge, and Noshin Menzies
Organisations: West of England and South West Academic Health Science Networks (AHSNs) and South West Neonatal Network
Published as part of the NNAP Annual Report on 2020 data
Share your own QI journey
Submit a projectReferences
Doyle LW, Crowther CA, Middleton P, Marret S, Rouse D: Magnesium sulphate for women at risk of preterm birth for neuroprotection of the fetus. The Cochrane database of systematic reviews 2009(1): Cd004661.
Crowther CA, Middleton PF, Voysey M, Askie L, Duley L, Pryde PG, Marret S, Doyle LW; AMICABLE Group. Assessing the neuroprotective benefits for babies of antenatal magnesium sulphate: An individual participant data meta-analysis. PLoS Med. 2017 Oct 4;14(10):e1002398
Lea CL, Smith-Collins A, Luyt K. Protecting the preterm brain: Current evidence-based strategies for minimising perinatal brain injury in preterm babies and improving neurodevelopmental outcomes. Arch Dis Child Fetal and Neonatal. 2016 Dec 23. doi: 10.1136/archdischild-2016-311949.
Burhouse A, Lea C, Ray S, Bailey H, Davies R, Harding H, Howard R, Jordan S, Menzies N, White, Luyt K.Preventing cerebral palsy in preterm labour: a multiorganizational quality improvement approach to the adoption and spread of magnesium sulphate for neuroprotection. BMJ Open Quality 2017;6:e000189.
National Institute for Health and Care Excellence (2015) Preterm labour and birth. NICE guideline (NG25). 2015.
Health Foundation Scaling-up Improvement award. https://www.health.org.uk/improvement-projects/precept2-reducing-brain-injury-through-improving-uptake-of-magnesium-sulphate
Finding the best way to scale up a perinatal Quality Improvement initiative: The PReCePT study. https://arc-w.nihr.ac.uk/research/projects/preventing-cerebral-palsy-in-pre-term-babies-the-precept-study/
Saving Babies Lives Care Bundle. Element 5, p38 https://www.england.nhs.uk/wp-content/uploads/2019/07/saving-babies-lives-care-bundle-version-two-v5.pdf
