Project PEEP: Introduction of a Preterm Respiratory Care Bundle on NICU
Establishing a team of interdisciplinary individuals to develop strategies to reduce the incidence of bronchopulmonary dysplasia on the neonatal intensive care unit through implementation of a preterm respiratory care bundle.
Background
A quality improvement (QI) team of enthusiastic interdisciplinary individuals was formed to develop strategies to reduce the incidence of bronchopulmonary dysplasia on our neonatal intensive care unit. We planned to achieve this through implementation of a preterm respiratory care bundle, primarily focusing on reduction in delivery room intubation and emphasis towards non-invasive ventilation and less invasive surfactant administration (LISA).
Improvement plan
Rates of bronchopulmonary dysplasia (BPD) or death as published by the national neonatal audit program (NNAP 2019) were 3.6% higher at our level 3 NICU than the national rate.
We planned to measure improvement using our database and badger net data to identify rates of babies intubated at birth, in comparison year on year through the QI process.
We sought to identify and compare oxygen requirement at 28 days as a possible early indicator of improvement in BPD incidence, with the intention of evaluating true BPD rates at the end of the year 2021.
The strategy was comprised of 4 cycles:
- Cycle 1 involved training staff in using LISA
- Cycle 2 implemented this technique
- Cycle 3 introduced delivery room nasal CPAP (DRCPAP)
- Cycle 4 focused on staff training in using video-laryngoscopy
Outcomes
Overall, there was an increase in respiratory support days, primarily non-invasive.
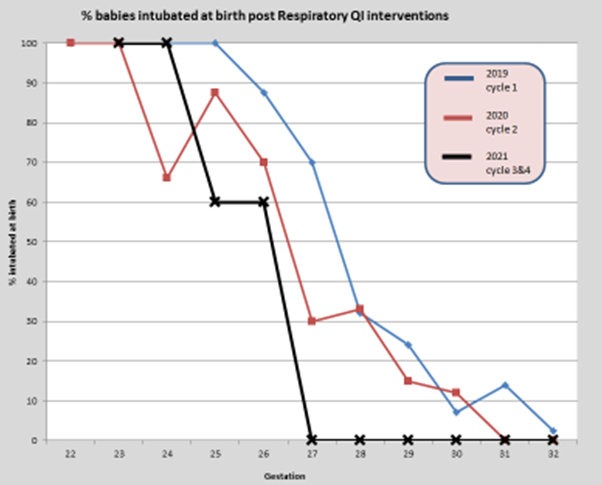
The care bundle has seen an overall reduction in delivery room intubation for babies born under 32 weeks gestation (see figure 1). This reduction is more noticeable between 27-32 weeks gestation as over the 4-cycle period the rates of intubation decreased from 70% to 0%. Between 25-27 weeks our rates of delivery room intubation have reduced by approximately 30-40%.
Preliminary analysis of rates of oxygen beyond 28 days has dropped by almost half for babies between 27-32 weeks gestation during the QI intervention period.
Successful implementation of QI methodology facilitating the introduction of a preterm respiratory care bundle has resulted in a significant decrease in the number of babies intubated at birth, potentially positively influencing the rate of BPD. We believe the care bundle has promoted standardised assessment and planning of care rather than care based on gestational age or personal bias.
The graph below shows % babies intubated at birth post respiratory QI interventions:
Top tips for implementation
We have found that inclusion of all members of the interdisciplinary team has helped significantly with adoption of practices, however the acceptance of change in practice for some of the more senior members of the nursing team remains one of the biggest challenges.
In hindsight a more stepwise approach to application of the practice changes per gestational age might have had a more convincing effect, however this would be difficult to achieve in a timely manner.
Authors: Lucy Bradley ANNP; Dr Teim Eyo, Jo Jones, Zara Grandison, Yvonne Huskins, Dr Nitesh Singh
Organisation: Neonatal Intensive Care Unit, University Hospitals Coventry and Warwickshire NHS Trust
Published as part of the NNAP Annual Report on 2020 data
