Snuggle and PEEP – Increasing use of non-invasive respiratory support and reducing bronchopulmonary dysplasia rates
This QI project aimed to increase the use of non-invasive respiratory support and reducing BPD rates.
Publication date: 12 October 2023
Authors
Emma Liggett (ANNP), Kirsty Lomax (ANNP), Ailish Davis (ST2), Doone Boorman (3rd year medical student), Adekunle Sobowale (ST4), Hannah Spierson (Consultant Neonatologist) Neonatal Unit, Bolton Hospital NHS Foundation Trust.
Background
Nationally, 39.7% of infants <32 weeks develop Bronchopulmonary dysplasia (BPD) or die (NNAP 2020-2022). However, our local data was nearly 10% higher at 48.2%. Our unit’s Getting It Right First Time (GIRFT) report identified that we had higher intubation rates in preterm infants in comparison to national data (49.4% vs 41.3%). Our baseline data highlighted that most intubations occur in the delivery suite.
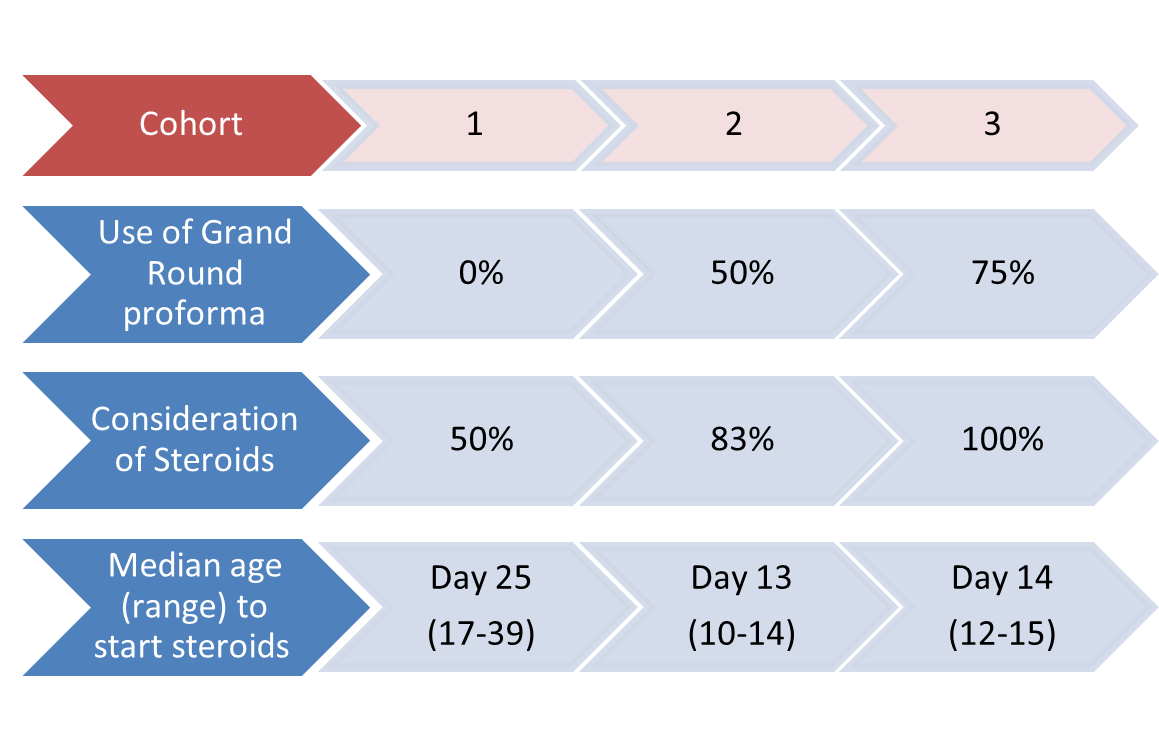
Although the development of BPD is multifactorial, we know that ventilator- induced lung injury is a significant contributory factor. Our baseline data also identified that postnatal steroids were only considered in half of eligible babies and were given late (Figure 1).
Figure 1: Postnatal steroids: Improvement over time
Measures
Eligible babies were those born at less than 32 weeks’ gestation in our unit. We collected data for three cohorts of babies to monitor progress over time:
- Cohort 1 – Baseline data – Born January to June 2021 – 34 babies.
Cohort 2 – Born October to December 2022 – 25 babies.
Cohort 3 – Born January to March 2023 – 25 babies.
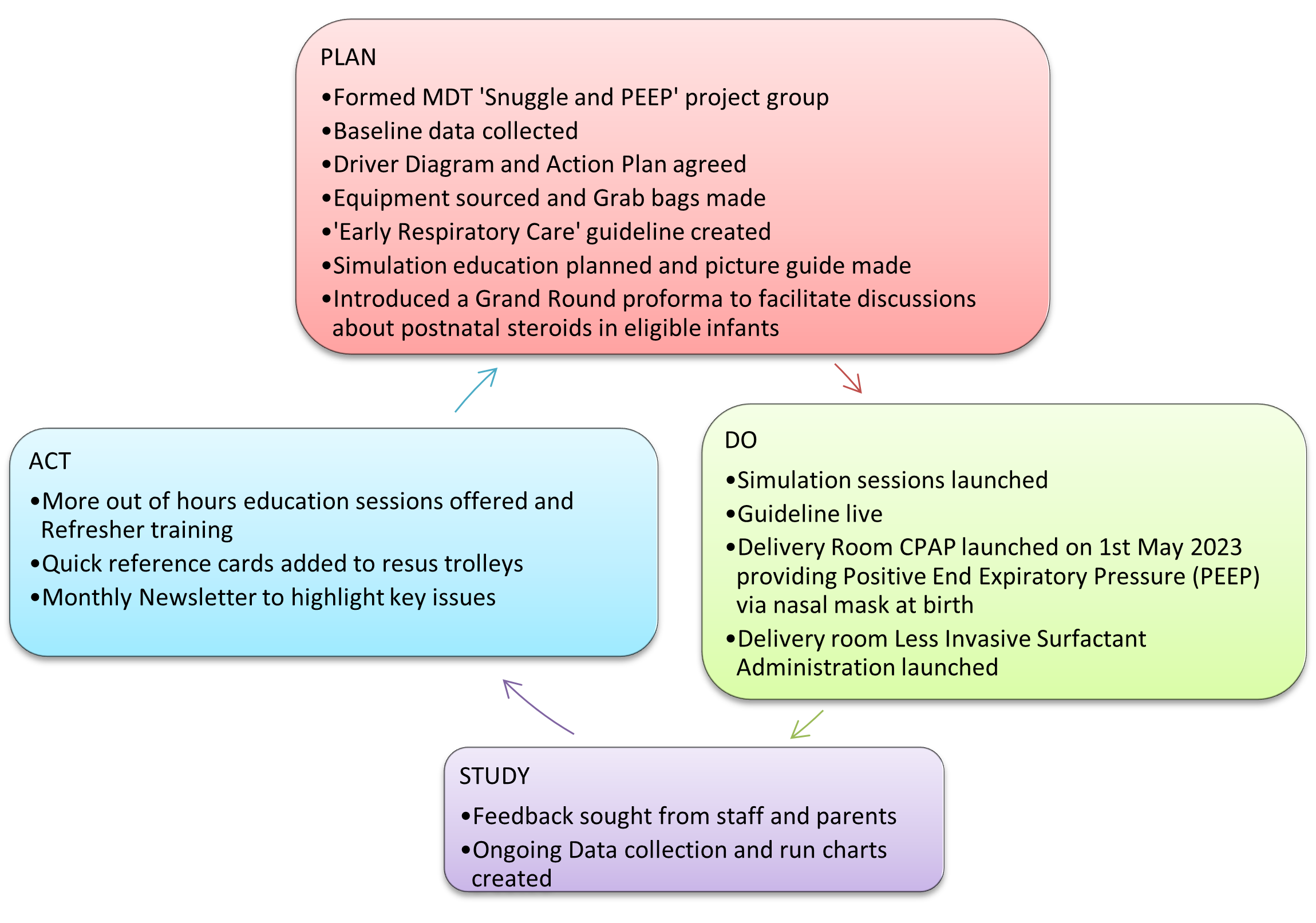
Figure 2: Our improvement plan PDSA cycle
Outcomes
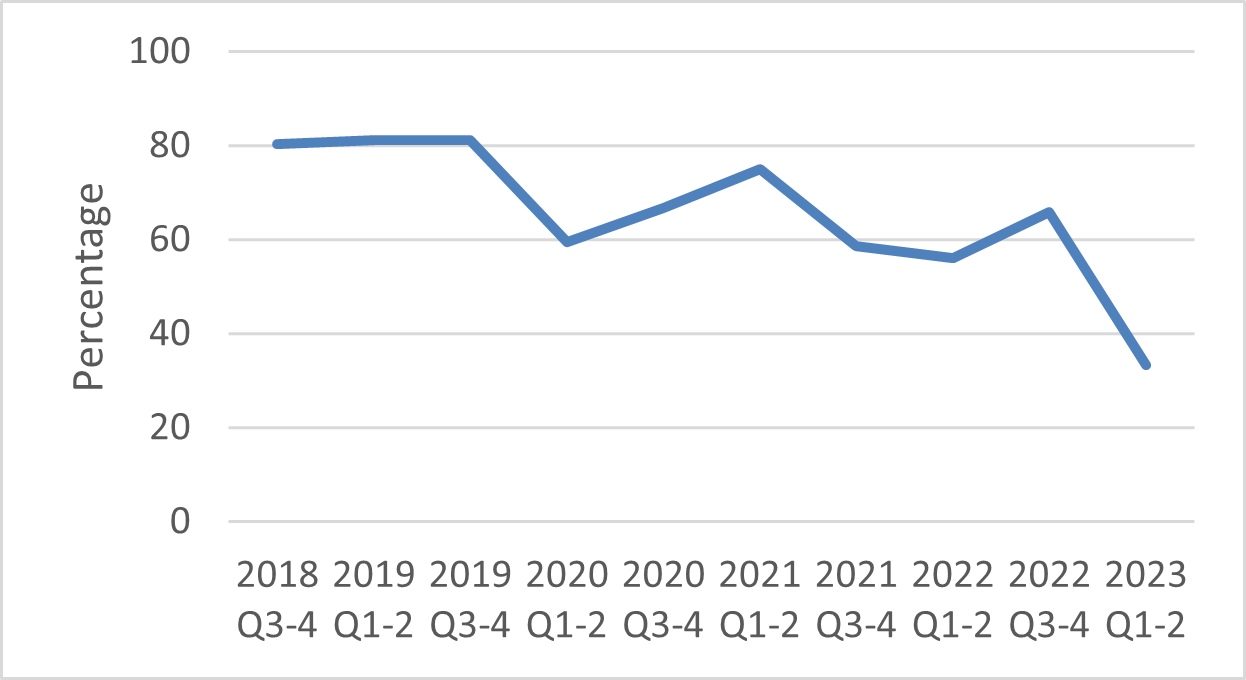
Our primary aim was to reduce intubation rates. Our intubation rates for <32 week infants at birth decreased from 68% in cohort 1, to 46% in cohort 3. We are expecting further reductions now that delivery room continuous positive airway pressure (CPAP) has launched. In babies who are ≥27 weeks, intubation rates (at any time) decreased from 69% in cohort 1, to 13% in cohort 3. Figure 3 shows our intubation rates of preterm babies (<32 weeks) in the first week over the last 5 years has decreased from 80% to 34%.
Figure 3: Percentage intubated in first week, 2018-2023
Staff feedback following delivery room CPAP was collected and included comments such as “all went smoothly, it was perfect for this baby”. A parent survey was undertaken 2 months after the introduction of delivery room CPAP. Longer tubing and a secured nasal mask allows for hands-free cuddles before transfer to the NICU. Following the introduction of delivery room CPAP, delivery room cuddles increased from 0% to 80% and opportunities for delivery room photos increased from 33% to 80%.
Baseline cohort parents told us their babies were “taken straight away”. Parents of babies who received delivery room CPAP were all positive about their delivery room experience. For example: “Amazing! An experience I didn’t think we would be able to have… he was brought over to us and passed straight to me for cuddles. The neonatal team were excellent about going to get my partner’s phone and capturing that special moment for us all. Amazing 5 minutes and exactly what Mum needs”. Further parental experience from the delivery room CPAP group is shown in Figure 4.
Figure 4 Parent experience word cloud, delivery room CPAP cohort group

We believe the MDT project group was key to our success, enabling us to drive training and develop resources effectively. Shift patterns and clinical workload limited staff attendance at simulation training. Therefore, we adapted our training and completed multiple shorter sessions in the clinical environment, including out of hours sessions. We also offered refresher training. A further challenge was some anxiety from staff regarding our new practices and equipment. The Snuggle and PEEP group attended preterm deliveries, to support the team during the delivery room CPAP launch, which helped assuage concerns.
Top tips for implementation
We found it beneficial to take time to understand our unit’s data and areas for improvement before introducing any new interventions. By regularly sharing data with the wider team, this helped raise awareness and build support for the project. We developed a guideline that was right for our unit and increased buy-in from the team.
Acknowledgements
Previous members of the Snuggle and PEEP group are Dr Harriet Wayman, Dr Khalida Yasso, Dr Eleanor Hunter and Dr Lucy Hoskyns.
