POSH: Prevention of Significant Hypothermia
This QI project began in response to suboptimal numbers of preterm infants being admitted hypothermic (<36.5c) to the NICU.
Authors
Lucy Bradley and Helen Cockcroft, two Advanced Neonatal Nurse Practitioners at University Hospitals Coventry and Warwickshire
Background
Preterm hypothermia is associated with significant morbidity and increased mortality [1]. The Prevention of Significant Hypothermia (POSH) group was created in response to suboptimal numbers of preterm infants being admitted hypothermic (<36.5c) to the NICU.
All members of the perinatal multidisciplinary team were consulted and involved in root cause analysis, resulting in creation of a driver diagram. Probable causative factors were identified as multifactorial and likely a combination of several influences rather than one singular issue.
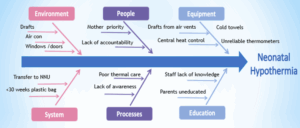
Figure 1. Driver diagram showing factors leading to Neonatal Hypothermia
Measures
Through QI methodology, four consecutive plan-do-study-act (PDSA) cycles have been completed, each related to a change idea identified following development of a driver diagram.
Interventions were introduced in cycles in order to establish effectiveness but also to allow the opportunity to ensure practices were fully embedded before moving on to the next change cycle.
Data was collected via Badgernet which assisted in determining location of birth and its relation to admission temperature, along with any specific causes / trends/environment. A monthly review of temperatures was published and discussed at daily safety huddles within the neonatal unit and labour ward highlighting both good and poor performances
with the objective of increasing awareness and accountability.
Our improvement plan
- Cycle 1: EDUCATION: Targeted Training packages, induction teaching, power points, visual displays.
- Cycle 2: ENVIRONMENT: Ventilation draft covers, towel warmer in theatres, Do Not Enter signage, room thermometers, baby thermometers in grab bags.
- Cycle 3: SYSTEMS: Concept of thermal manager throughout stabilisation introduced to increase accountability. Normothermia checklist.
- Cycle 4: EQUIPMENT: Neohelp plastic bags, Continuous skin temp monitoring throughout stabilisation.
Outcomes
POSH intervention strategies using the BAPM QI framework for normothermia have significantly improved admission temperatures of babies born <34 weeks gestation.
Admission temperature within target range of 36.5-37.5c has improved from 58% (2017) to 88.5% (2023) with the implementation of POSH strategies for preterm deliveries <34 weeks gestational age. Our unit is now achieving positive NNAP outlier status for this measure.
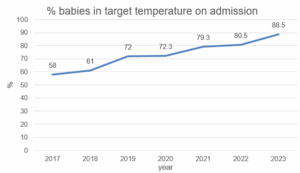
Figure two. Run chart showing percentage of babies achieving targeted temperature range on admission
Sustaining improvement has been achieved through regular monthly monitoring of admission temperatures and ongoing promotion of the QI project at daily safety huddles, safety champions meetings, and periprem review meetings.
Challenges and learnings
Continuous data monitoring allowed us to identify an unintended consequence during the POSH initiative, as there was an increase in the incidence of hyperthermia contributing to failure in achieving target temperature range in 2020. From December 2020 the use of continuous skin temperature monitoring throughout stabilisation was introduced to combat this issue. However, this resulted in a longer amount of time being taken to close the plastic bag following delivery thereby having a negative effect on thermal management. Consequently, repeated, regular axilla temperature monitoring and action throughout stabilistaion was implemented.
Furthermore, empowering the nursing team to take responsibility for thermal management at deliveries has seen increased involvement of the nursing team and a more proactive approach by all stakeholders.
Top tips for implementation
Ensuring a perinatal multidisciplinary approach has been vital to the success of this project.
Acknowledgements
Nil.
References
1. Perlman JM, Wyllie J, Kattwinkel J et al, Part 7: neonatal resuscitation: 2015 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015;132:S204-S241
