Improving HbA1c For Children and Young People Living With Diabetes
Improving the mean HbA1c for all children and young people living with diabetes who are treated with continuous subcutaneous insulin infusion using a package of support and education.
Our overall HbA1c was above the national average and therefore an outlier in the NPDA 2015/16.
A third (58) of our 167 children and young people with diabetes (CYPD) used continuous subcutaneous insulin infusion (CSII) as their treatment option. Despite using CSII technology, we identified that these patients had a mean HbA1c (63mmol/mol) similar to the mean of the entire CYPD (65mmol/mol) cohort. Usually we would expect this group to have significantly better outcomes, thus maintaining an optimum distribution of NHS resources, given the cost of this expensive technology.
Patients were therefore not using their technology to optimise blood glucose control, and thereby not reducing the risk of long term complications. Financially, there is both a short and long term impact for the NHS, in the immediate cost of an insulin pump as well as the cost of any future complications.
Causes of the Problem
We identified the following causes:
- Unclear and informal internal processes, both for commencing and continuing on a CSII.
- Patients and families were receiving inconsistent expectations for pump use and outcomes by different team members.
- Gaps in patients knowledge/education.
Project Aim Statement
Our aim was as follows:
To improve the mean HbA1c for all patients using CSII, by 10%, within 1 year.
Stakeholders
The project team consisted of:
-
- Dr Jai Ganapathi Consultant Paediatrician
- Dr Jasjit Bhandari Consultant Paediatrician
- Catherine Tapping PDSN
- Sharanjit Cheema PDSN
- Manpreet Mudher PDSN
- Phoebe Kurian PDSN
- Leah Brennan Clinical Psychologist
- Debbie Blissitt PDSD
Our stakeholders were:
- Dr Catherine Mitchell, Consultant Endocrinologist, involved in our transition clinic for those aged 16-19 years
- Victoria Conway, helping with data quality
- CSII patients
PDSA Cycles / Solution(s) Tested
We started with four PDSA cycles:
-
- Pump refresher
- Pump demo
- Pump support plan
- Pump start up process
A run chart was made to record HbA1c for all CSII patients.
A QI meeting time was agreed weekly and booked into all MDT team diaries.
PDSA Cycle 1 – Improve Attendance at Pump Refresher:
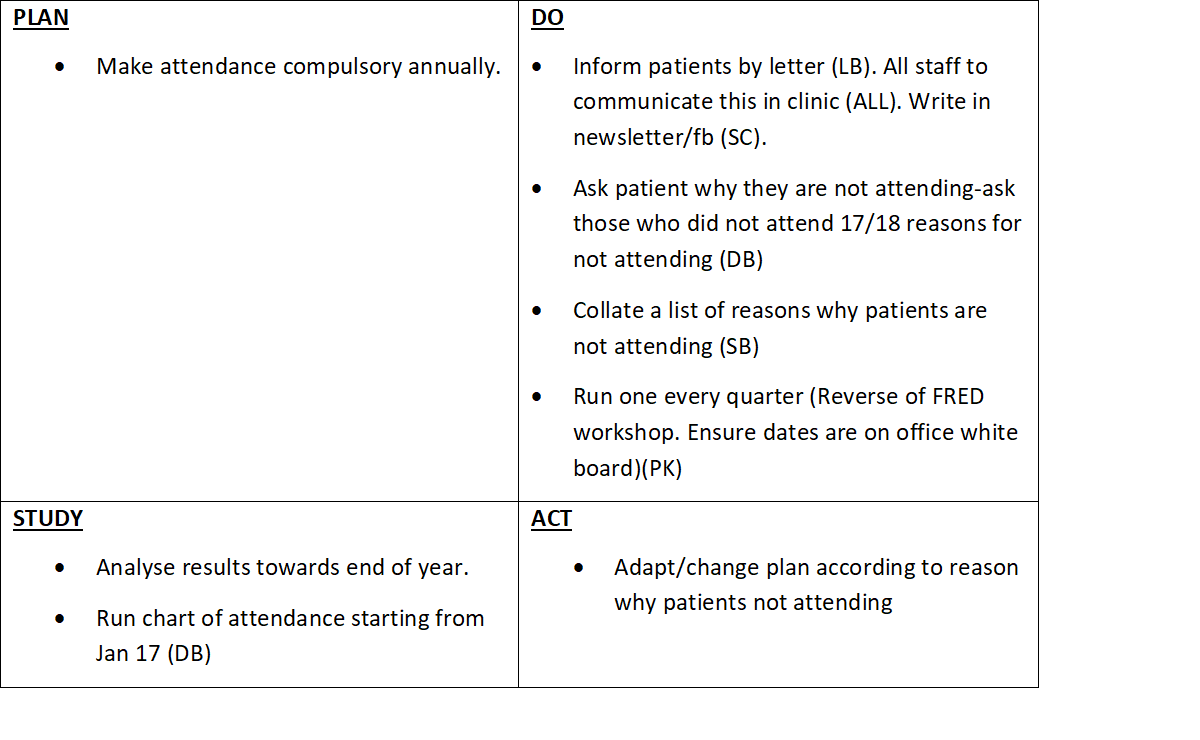
Feedback was used to re-write the education session, making it more interactive and updated annually.
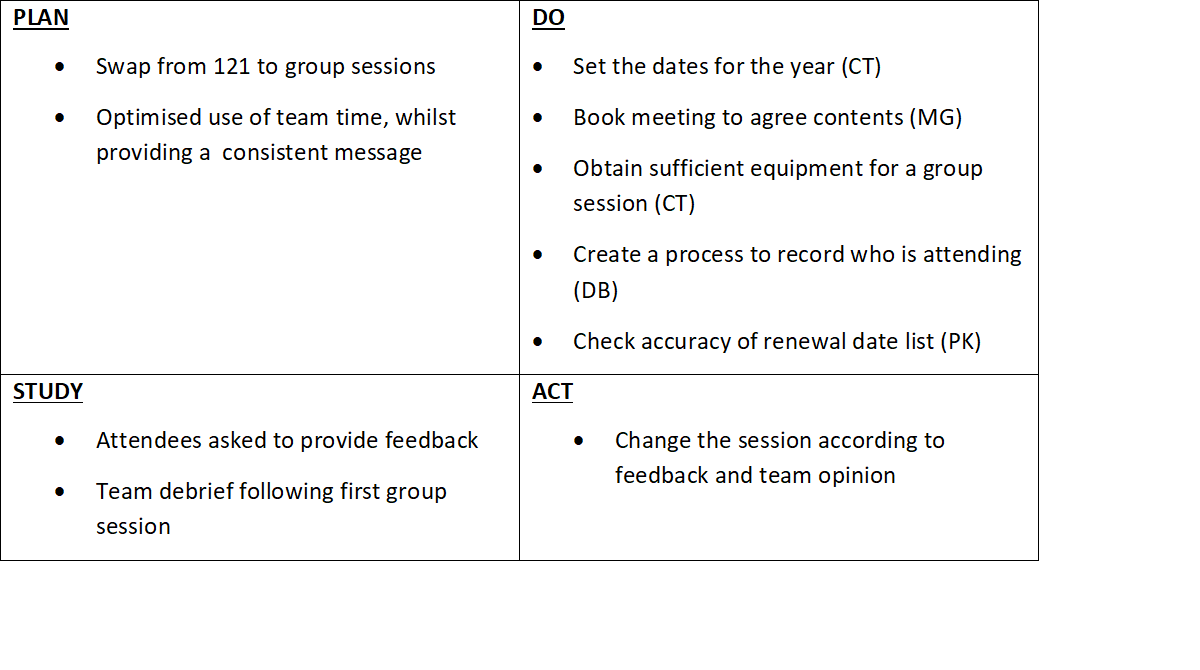
PDSA Cycle 2 – Pump Demo
PDSA Cycle 3 – Pump Support Plan (PSP)
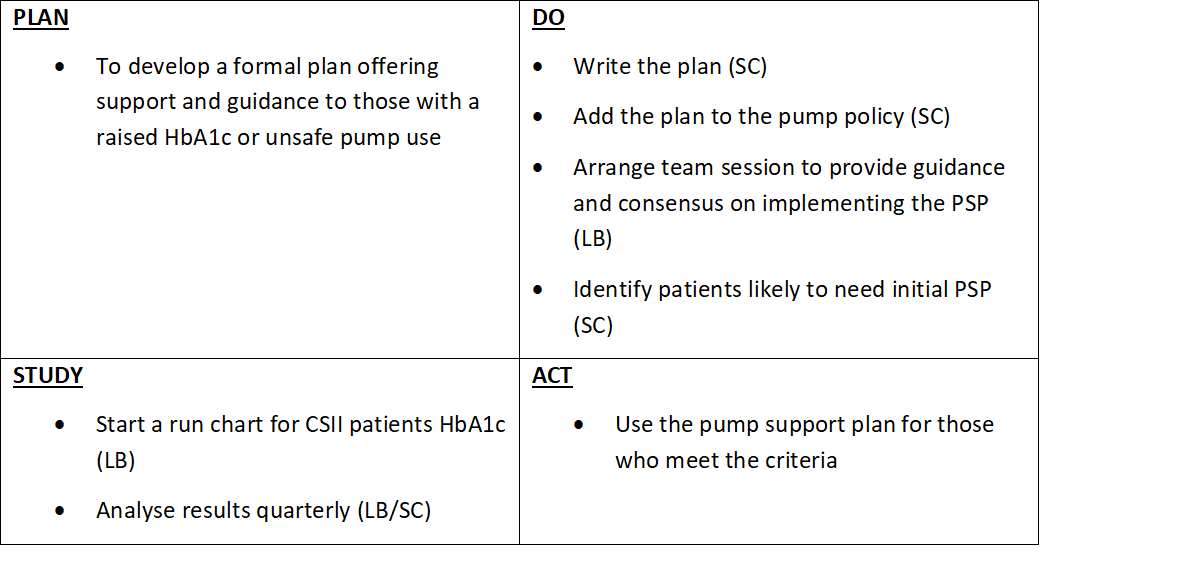
A template letter was developed to be completed in clinic, with the CYPD/family, and a copy to be given to them as well as one for the file.
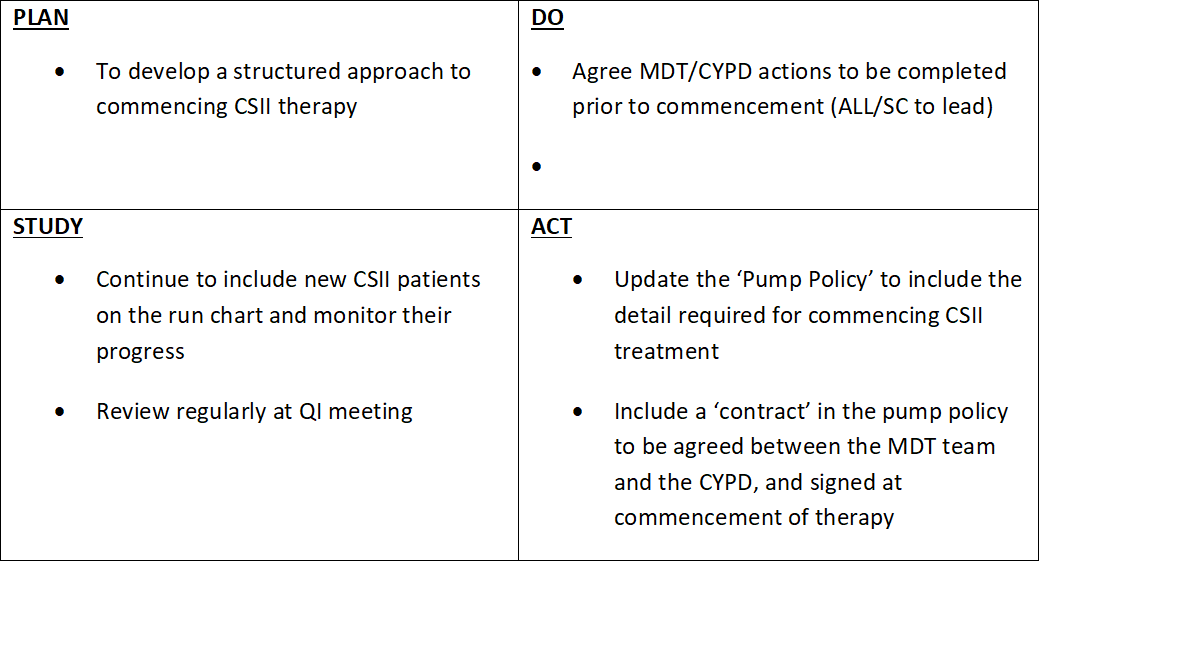
PDSA Cycle 4 – Pump Start Up Process
Data Results
Figure 1: Changes in the mean HbA1c of all CSII patients
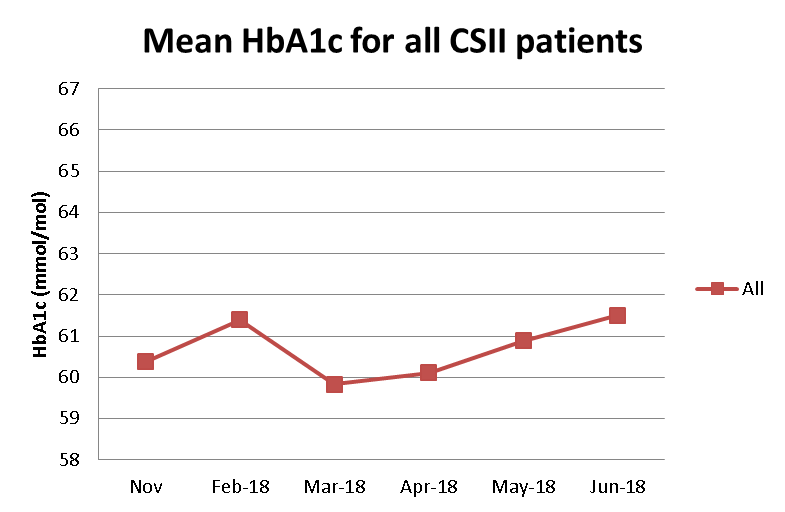
Figure 2: Changes in HbA1c comparing PSP and non-PSP groups
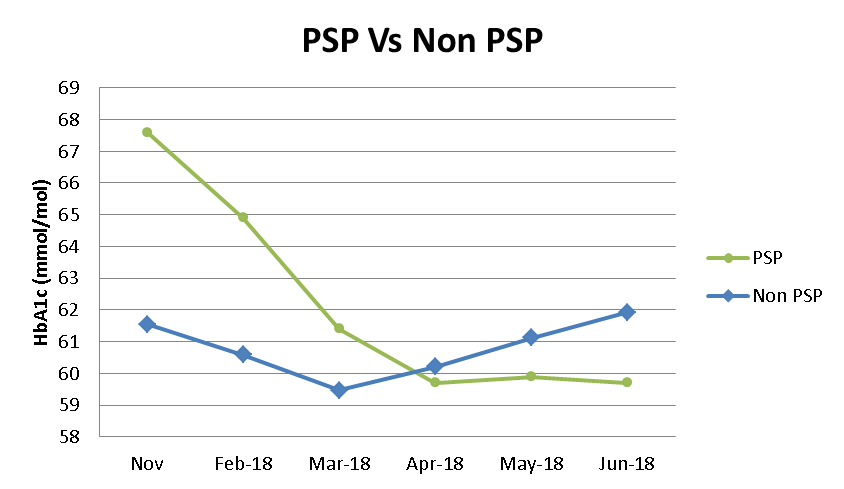
Figure 3: Changes in HbA1c at individual patient level

How This Improvement Will Be Sustained
Pump refresher dates are booked, four per year, at the start of each year:
-
- Patients are allowed to choose from the dates, however annual attendance is compulsory
- Staff meetings are arranged to plan each session
- Expectations for pump use and PSP are included in this session
Pump demo dates are booked, four per year, at the start of each year:
-
- Patients considering starting CSII are invited to attend, alongside those due for pump renewal
- Pump contract is discussed at each session so patients are aware of what would be expected of them, including annual attendance at pump refresher
At pre clinic meetings the team discuss patients who may need to be started on a PSP.
A new pump policy has been developed. This includes:
-
- A signed contract between ourselves and the patient summarising expectations of pump management and patient engagement with the team
- A list of actions that patients must complete prior to starting on a pump, including attendance at a pump demo session
Challenges and Learnings
What would we do differently:
- Involve the team administrator from the outset
Secrets to success:
- A cohesive and motivated team
- Allocated QI time
Suggestions for Further Implementation
This QI project shows that consistent team messaging on criteria for device continuation and explicit contracts with carers does help improve outcomes. This can be adapted to other teams where messaging needs to be consistent to improve outcomes.
Project Lead: Dr Jai Ganapathi
Organisation: The Hillingdon Hospital
Published: May 2019
