Establishing Paediatric Trainee Clinics During the COVID-19 Pandemic
Redesign of outpatient clinics delivered by paediatric trainees during the COVID-19 pandemic to incorporate telephone and video consults with some continued face-to-face consultations.
Paediatric trainees delivering outpatient clinics provides a valuable learning opportunity and forms part of the Royal College of Paediatrics and Child Health (RCPCH) postgraduate paediatric training curriculum. During the COVID-19 pandemic, outpatient clinics have been redesigned to incorporate telephone and video consults as well as continuing some face-to-face consultations. The NHS Long Term Plan also advocates the use of digitally enabled care.
The Problem
The pandemic and the resulting rapid change in outpatient service provision resulted in registrar clinics being halted. Consequently, there was a loss of registrar training experience and reduction of clinic numbers.
The paediatric training programme comprises an annual review of competency progression (ARCP) which is the means by which doctors are reviewed each year to provide safe and quality patient care. One of the standards in the West Midlands School of Paediatrics includes the recommendation of attendance to at least 10 outpatient clinics yearly. We conducted a short trainee survey at Birmingham Children’s Hospital (BCH) General Paediatric department of which 50% senior trainees at the registrar level had attended less than 5 clinics in the previous 6-month post.
Due to the current COVID-19 pandemic at Birmingham Children’s Hospital it was identified that 2 months into the current post 83% senior trainees had attended 0 or only 1 clinic. During problem analysis, rota shortages, shift patterns, being less than full time and other clinical commitments were identified as barriers to attending clinic as well as the limited outpatient activity occurring due to COVID-19.
Aims
- In a 6-month post, trainee should aim to attend 5 clinics. We had already identified 2 months into the current post that trainees had been unable to attend clinics so this was an ambitious target to achieve during the remaining 4 months but felt to be achievable.
- To devise trainee clinics such that it provides a useful learning opportunity with adequate time built in for consultant supervision and to enable work-based placement assessments to be undertaken.
- To develop trainee confidence in doing telephone or video clinics. This was crucial as following a trainee survey it was identified no trainee had done a telephone or video consult before and confidence on a rating scale was 5/10.
Stakeholders
Patients were given the opportunity to fill out a satisfaction survey following clinic. This was sent via text message link. Trainees were also asked to provide feedback via an online survey and consultants were asked for feedback via a semi-structured interview format. There was managerial involvement in setting up clinics and negotiation of consultant time re-imbursement for clinic supervision.
The clinics contributed to the department’s outpatient activity, and outcome measures also included length of clinical activities which was filled out prospectively.
PDSA cycles/Solutions tested
PDSA cycle 1
An initial 2-week pilot was commenced with involvement of 5 supervising consultants. The standard operating procedure (SOP) for how to run a registrar clinic was distributed to trainees along with a clinic rota and supervising consultant. The SOP included:
- step by step instructions regarding what to prepare before clinic
- how to conduct telephone and video calls
- how to dictate letters
Details of the SOP can be downloaded form this webpage below.
Trainees were advised to look at the virtual consultation guide on the intranet. For morning face to face clinics (08:45 until 13:00) there were slots for 4 new patients while the afternoon phone/video clinics (14:00-17:00) had 3 new patients booked and were conducted in consultant offices.
Time was allocated for discussion with the supervising consultant pre and post clinic. Administration time was built in and it allowed time for the trainees to get to grips with telephone or video clinics. The ‘AccuRx Fleming’ video calling system was used which is NHS digitally accredited and trainees were advised to practice using the test patient system.
A message patient facility could be used to send patients a link into the video appointment. They could then also send a text message to the patient with the patient satisfaction survey link.
PDSA cycle 2
The 2-week pilot was extended and clinical fellows were also included.
Regular monthly virtual meetings were set up to discuss progress and any problems arising. These included mini face-to-face individual sessions organised for some trainees finding the video system difficult to get to grips with. We devised easier access to the clinic rota for consultants, trainees and the operational manager via a common drive so clinics could be booked seamlessly when trainee and consultant availability was confirmed.
Not all computers used had cameras so it was identified on each date if the computer had a camera and availability to allow for video consultations to be undertaken.
PDSA cycle 3
An extra patient slot was added to the telephone/video clinics and changed to 2 new patients and 2 follow ups.
Outcome data
Improvements in trainee attendance at clinic
19 phone clinics and 12 face to face clinics were undertaken by trainees during the 4-month period generating a possible 106 appointments. During this time there were 7 did not attend outcomes. In addition, 2 patients cancelled and 2 patients were rebooked into different speciality clinics. The number of trainee clinics occurring monthly increased (table 1):

All the trainees that completed the rotation had achieved 5 or more clinic attendances even being less than full time (LTFT). 2 trainees did not complete the rotation due to change of job or redeployment back to community so as a result did not complete this target.
Improvements in learning with consultant supervision
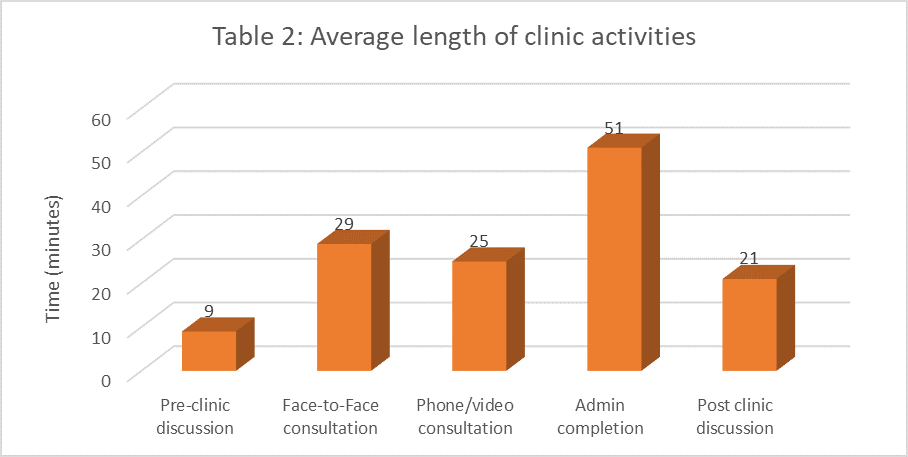
Average length of clinic activities revealed there was only a 4-minute difference between face to face and phone or video consultations. 14 requests for work-based place assessments were submitted although this number may be higher as 9 clinics had missing data. A breakdown of clinic activities is shown in table 2:
Developing trainee confidence in doing telephone or video clinics
Unfortunately, despite encouragement of the use of video consultations only 4 video consultations were documented. There were 9 clinics with missing data so it could be that some of these were video consultations and not documented.
It is also possible there is ongoing reluctance or uncertainty regarding the use of video as a consultation tool. Some patients were also reluctant to use video when asked on the phone and the appointment letters sent out did not specify that video consults maybe used over telephone. However, trainee confidence did increase:
Trainee survey:
- Confidence in doing a telephone or video consult increased to 8/10 on a rating scale from 5/10.
- All trainees felt adequately supported and would like clinics to continue.
- When asked about advantages or disadvantages some of the comments included ‘Different way of working and gaining experience in outpatient setting’, ‘Ease of patient/family to attend but missing out on interaction that face to face clinics may provide’, ‘It was difficult finding a computer with the mic and dragon (Dragon Winscribe is our dictation programme for clinical letters)’, ‘Found completing SLEs easier during clinic’, ‘offered video consults but all patients said no, can we add this to letter sent out?’.
Patient satisfaction survey:
- 9 responses of which 67% had a face-to-face clinic and 33% had phone/video clinic.
- 100% felt the doctor listened and concerns were adequately addressed.
- Patients rated 9/10 for satisfaction with appointment and overall experience.
- Additional comments included ‘The doctor was pleasant and all staff I dealt with’, ‘It was good’.
Challenges & learning
When we asked trainees about changes they would make, suggestions included ‘I would like to get experience doing video clinic as it’s more interactive and you can see signs and symptoms in real time which helps in diagnosis and management’, ‘Having a designated clinic space which doesn’t change from week to week and which you know will always be available for your virtual clinic’.
In practice encouraging trainees to do more video consultations rather than telephone has been challenging. Ideally during the next rotation this will be reinforced at induction and more face to face training may be needed. Clearer appointment letters explaining video consultation may also encourage more patient participation.
Initially trainees were good at filling out the data prospectively but this became more difficult with missing data as a consequence. Although extra time was built into clinics some trainees had challenging clinics due to complex patients. The plan is to change this and have consultants identify who is suitable for trainee clinics during the triage process.
A small number of patient satisfaction surveys were filled in. This will need to be changed to a validated patient questionnaire to make the results more reliable.
Consultant feedback from semi-structured interviews included:
- ‘Supervising trainee clinics remotely easier and not too much added work’.
- ‘Letters are done in clinic. Smoother, efficient and more manageable’.
- ‘If workload was more spread amongst team would be less work’.
- ‘Some trainees may not have read SOP thoroughly as many answers regarding clinic working in there already’.
- ‘Some trainees still feel nervous doing video consults.
- ‘Found watching trainee do a video consult interesting/enjoyable’.
- ‘Outpatient work underrated in terms of training experience but bulk of work as paediatrician’.
- ‘Debrief before and after helps. Supervision time built in which have never had before’.
- ‘Could be a springboard to other trainee opportunities – grading referrals.
- ‘Great experience’.
- ‘Telemedicine will be the new normal’.
How this improvement will be sustained
During each rotation managing trainee clinics will be given as a task to a trainee. This will help to ensure continual sustainability. Encouraging other consultants to participate in supervision will also help to sustain clinics. Currently there is a proposal for consultant reimbursement of time for supervising a registrar clinic. The proposal is that for each clinic supervised 2 follow-up patients are taken from the supervising consultants follow-up waiting list and the consultant also sees 2 less new patients in their clinic.
Suggestions for further implementation
Birmingham Children’s Hospital is looking at redesigning the whole outpatient service to incorporate telemedicine.
Project Leads: Dr Amrit Dhesi, Dr Ranvir Dhoot, Dr Lisa van Geyzel, Dr Helen Morris, Dr Robin Tall, Dr Esai Archary, Dr Catherine Tyler
Organisation: Birmingham Children’s Hospital, Steelhouse Lane, Birmingham, B4 6NH
Published: December 2020
