Establishing The Hillingdon Community Joint Neonatal Clinic During COVID-19
An initiative by the neonatal team at Hillingdon Hospital in response to the challenges of delivering specialist care during the COVID-19 pandemic and its impact on very young babies and their families.
On March 27, 2020, at the start of the COVID pandemic, The British Prime Minister and the Member of Parliament for Uxbridge and South Ruislip asked the entire country to enlist in the war against COVID-19 pandemic. He said, ‘Stay at Home. Protect The NHS. Save Lives.’ This directive has transformed the way we deliver health care in the NHS.
The Problem
The Neonatal Unit at Hillingdon Hospital is a twenty-cot local neonatal unit in The North West London Operational Delivery Network that provides short term intensive care for sick new-born babies and long-term high dependency and special care for early, moderate, late preterm and term babies. About 400 babies are admitted to the unit each year delivering a total of 182 intensive care days, 1192 high dependency days and 1879 special care days in 2019/20. In 2016, the unit established a transitional care ward co-located on the postnatal ward for short term admissions of term and late preterm babies.
Most of these babies will require a follow-up appointment with a neonatal paediatrician once discharged from hospital. The service runs several clinics each week for babies and their families to review their growth, their development and how they are adjusting to life in the community. These consultations are vital for the well-being of these babies who are at a critical phase of their early development.
The instruction to stay at home and the introduction of the two-metre physical distancing rule led to a decision by The Trust to limit the number of patients attending outpatient clinics to about 20% of the total clinic list. In addition, parents heeded the public health advice and reported that they felt very unsafe bringing their very young babies to hospital for appointments. These measures caused significant disruption to the delivery of our neonatal outpatient service. It meant that many babies could not be reviewed physically by a clinician. Telephone and video consultations were introduced but many parents fed back that it was a poor substitute to physical contact.
Aims
At a meeting of the Neonatal Management Team during the early months of the lock down, clinicians resolved to explore ways to increase access to clinic visit consultations. One of the options that was agreed was to seek partnership with external partners to source venues where specialist neonatal clinics could be conducted face to face safely. A potential negotiating position was to highlight the benefit to community services of a joint clinic with health visitors. One of the partners we approached was the local council. The London Borough of Hillingdon has an extensive network of Children’s Centres used as a great resource by families of children at a critical phase of their early development to access local services and reduce isolation.
The aim of this project was: To develop and conduct face to face clinics for appropriate Neonatal Unit graduates jointly with a health visitor in a Local Authority Children’s Centre facility.
Stakeholders
The Borough’s Children’s Services Department oversee a number of statutory services locally for children. Some of these include safeguarding children and the Children’s Centres. Children Centres were set up about 12 years ago to cater specifically for children in their early (0-5) years. The first year is considered a critical phase in early development and services are usually configured to cater for the needs of babies and their families in this age bracket. Within these centres are play facilities for children, access to resources such as breastfeeding and infant feeding classes, maternity classes, post-natal classes, or access to experts such as paediatric therapists
Since 2018, the Local Authority Children’s Services has taken on the commissioning of health visiting services. Health visitors that care for the children in the borough are employed and managed by Central and North West London NHS Foundation Trust. Many health visitors use these centres for well-baby clinics, providing advice for families, support, regular weighing and referrals at drop-in or scheduled appointments. Children’s Centres are well established as a community resource but had very few links with the local hospital based paediatric services.
The Department of Paediatrics at Hillingdon Hospital has twenty consultants, each with an area of interest and expertise. Five consultants oversee the Neonatal Service. In 2017, the department embarked on an award-winning initiative in collaboration with the Local Clinical Commissioning Group. Each week, several consultants conduct clinics jointly with General Practitioners at local surgeries. This initiative was welcomed by the local families and general practitioners and had always received high levels of satisfaction from users.
Other community paediatric services operating out of GP practices included the paediatric asthma services, paediatric diabetic service and paediatric allergy services. This shift to community-based services has significantly improved the health outcomes of children, eased access to specialist paediatric expertise in the community settings and reduced waiting times for children and their families. In addition, the failure to attend clinics rates were lower, reducing waste. The success of these community-based specialist clinics with local families proved that they can be run successfully outside usual hospital outpatient settings provided appropriate safeguards (COVID-19 secure) were put in place.
PDSA cycles/Solutions tested
The combination of COVID-19 pandemic lockdown, the introduction of physical distancing in public spaces, the decision of families to heed the Public Health messages and avoid hospital attendance coupled with the professional anxiety that children at critical phases of their development were not accessing care, moderated whatever barriers the Borough’s Children’s Services Department and Hillingdon Hospitals NHS Foundation Trust may have had to working together.
The Council agreed there was a need for hospital paediatricians and health visitors to work together to support vulnerable children and their families and minimise the sense of isolation felt by most families. The Trust’s paediatricians acknowledged that a significant proportion of ‘graduates from the Neonatal Unit’ would benefit from the combined expertise of both hospital-based and community-based clinicians. Both professionals working together will add value to any consultation, provide advice and support, and by intervening early when necessary improve health outcomes for these vulnerable babies.
The idea of a joint community neonatal clinic was discussed at a meeting at the Palace of Westminster with one of our local MPs, Rt Hon David Simmonds, formerly Deputy Leader of the Hillingdon Council until December 2019 when he was elected to his seat at the House of Commons as Member of Parliament for Northwood and Pinner.
Following the meeting, the Local Authority gave approval for the setting up of a joint clinic for babies discharged from the Neonatal Unit at a Children’s Centre. This decision was announced at a conference between the hospital clinician, the health visiting manager and the borough’s commissioner for children services in October 2020. The Regional Manager for the Children’s Centres was tasked with working with the hospital and health visiting teams to iron out the details of the programme.
Planning a Neonatal Clinic at a Children’s Centre
There are several Children’s Centres in the Borough. During negotiations with the Regional Manager, we discussed the facilities available at each centre, the floor space available, the times when the facilities were open and the distance from the hospital. It turned out purely by chance, that Colham Manor Children’s Centre ticked all the boxes as the most suitable venue for the Children’s Centre Community Neonatal Clinic.
It was available on the day and time when the hospital neonatal clinics were run. It had two rooms that we could use – one to use as a waiting room for parents (ensuring physical distances are kept) and weighing the babies, and the other for conducting the consultations. In keeping with COVID-19 secure guidelines, the rooms were large enough to accommodate a mother with her buggy, the baby, a clinician, and a health visitor.
The facility also had other equipment for example a digital audio visual screen for teaching, Wi-Fi to connect families if some training or education sessions was required and a play area for children if they attended the clinic. The centre also has a play garden where in warm weather children and their families could interact.
The Centre Manager was clear that whilst the rooms and building was available to use, they could not provide the specialised equipment that was necessary to run a neonatal clinic smoothly. As a centre it had a weighing machine and a table for changing babies. It was the responsibility of the hospital team to provide whatever equipment they required. The facilities at the centre were impressive and there were adequate safeguards to keep babies, their parents, and staff safe.
Conducting a specialised clinic in a Children’s Centre is a herculean task. For one, the hospital paediatrician is in an unfamiliar environment and what is taken for granted in a hospital environment required careful thought and risk assessment in the community. The neonatal clinicians determined that only babies with a particular risk profile should be scheduled to attend these clinics. They were also the babies who stood to benefit the most from the expertise of the health visitor who will be jointly hosting the clinic.
A standard operating policy document was produced detailing everything that needed to be done for the clinic to be safely conducted. This document included lines of responsibility for children if one became unwell suddenly whilst visiting the centre. We also considered in the document which agency should handle a complaint if one was made as three organisations were collaborating to run the clinic. One rewarding outcome from this exercise was the agreement that the letter inviting a child to the appointment should have the letterhead of the Hospital and the Local Council. We also agreed to obtain feedback comments from the families who attended the clinic.
Developing a Digitally Enabled (Paperless) Clinic
This clinic was conceived and planned in the COVID-19 era when a lot of our activities had been transferred to the digital space. It made sense that the new clinic should adopt a digital framework as rapidly as possible. We engaged with the Trust IT solutions team to allocate a Clinic Code and develop an online digital proforma to serve as the clinic consultation document. The Trust has an online database developed in partnership with the local clinical commissioning group that enable relevant clinical documents to be accessed easily. Neonatal documentation was easily accessed through the online Standardised Electronic Neonatal Database and Health Visitors had a unique database for clinical records. We also worked with the Trust’s Pharmacy Department to develop an e-prescribing programme for the clinic. These online platforms could all be accessed via a secure Wi-Fi connection.
The Hospital Outpatient Department had an online language translation service that could be accessed easily by telephone as well. The vision for this brand new community joint neonatal clinic was for it to be fully ‘paperless’. With the support of the Trust management, several of the relevant resources for a digitally enabled clinic were in place by the time of the first clinic. One important equipment for the clinical team was also the provision of a personal laptop for the hospital paediatrician to access the databases online using the Wi-Fi connectivity at the Children’s Centre.
Conducting the First Joint Neonatal/Health Visitor Clinic at a Children’s Centre
The day started brightly enough and soon became cloudy and rainy, but this did not dampen the enthusiasm of the families, staff of the centre, the health visitor or the visiting paediatrician. The health visitor and the paediatrician were at the centre and all set up before the first patients arrived. The Paediatric Outpatient Administration Team had prepared a large box of all conceivable equipment and paperwork that would be needed to conduct the clinic.
The first patients were welcomed by the centre manager and shown to the waiting room which has been cleaned and sanitised. The clinicians gloved, gowned, and wearing googles weighed, measured, documented, and plotted their growth charts before moving them to the large consulting room (Figure 1). The surfaces were cleaned down after each child and gloves changed. The consultation then took place and the babies were examined on another surface that was re-sanitised afterwards.

Figure 1: Paediatrician & health visitor with a baby and parent at the Community Neonatal Clinic.
During each consultation there was discussion between the parents, the health visitor and paediatrician about the right course of care for families to take. There was a real partnership in the meeting – every one’s experience and expertise acknowledged and included in the mix. Decisions were made and for some children an electronic prescription was filled and forwarded to the hospital pharmacy department. At the conclusion of the consultation, arrangements for follow up appointments were agreed, and the parents invited to provide some feedback. To accommodate the times for weighing and dressing, each appointment was scheduled to last 20 minutes. This worked quite well and indeed everyone kept to the time allocated and the clinic finished on schedule.
Outcome data
100% of the children and their families invited to the clinic attended. 100% of the parents completed a questionnaire inviting feedback about their experience.
Feedback from families
All the families that attended the clinic gave feedback on their experience. The feedback was excellent: From the organisation of the clinic, the welcome they received at the Children’s Centre and the professionalism they experienced from the clinician at their consultation.
They responded positively to the question on whether they would recommend the clinic to other families. Each of the attendees chose to return for a clinic visit appointment at the Children’s Centre for their next appointment rather than accept a telephone or video enabled consultation. Specifically, all the parents stated they ‘agreed’ or ‘strongly agreed’ with the statement; ‘The consultation with the professionals felt safe for me and my child’ (Figure 2).
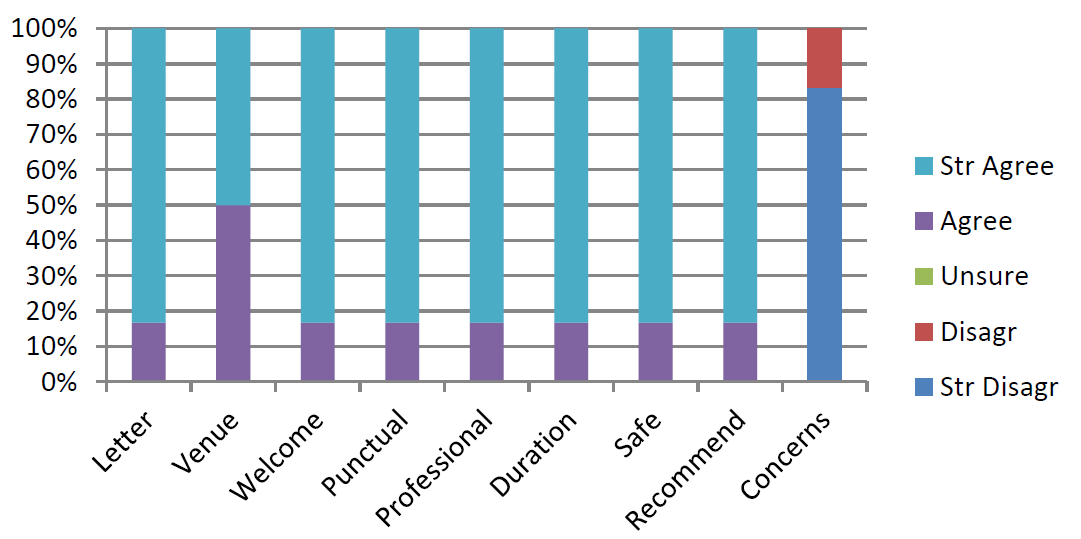
Figure 2: Responses to feedback questions
All the parents (100%) who attended also gave free text feedback:
- ‘Staff is really nice and helpful. They are very nice to me and I feel safe there’
- ‘Thank you so much for your help. The staff was very kind and helpful’
- ‘Thank you for your help and support’
- ‘The experience was great; I would recommend other families attending this clinic Thank you for your help and support’
- ‘We are so grateful to have been able to have a F2F review for our girls and the clinic felt very safe’
Challenges & Learning
Any Trust embarking on a similar project:
- Must nominate a clinical champion who must be supported by the Trust Management and introduced to key officers in partner organisations.
- Must involve the Outpatient Service Team from the outset – they know about clinic codes, costs, note pulling, outcome data and other details of an efficient outpatient service.
- Should engage the IT services early on to understand the infrastructure needed for an IT enabled community based paediatric clinic.
- Must ensure that it is resourced as you would for an outpatient service with appropriately trained staff, relevant equipment and adequate funding.
- Must consider the lines of responsibility for comments, complaints and commendations as more than one organisation is involved in running the clinic model that we have developed.
- Should consider other ways to provide value for the staff and families during the visit eg facilitating peer led health education classes or specialist sessions (e.g. infant feeding clinic) for families.
How this improvement will be sustained
- It is important that there is buy in from the whole clinical team and the management team. The service must be available and used by all members of the team.
- The service must be commissioned by the Trust and partner organisations to ensure that appropriate resources are allocated to the running and development of the clinic.
- The service must be audited regularly and inspected by relevant regulatory agencies in health and social care to ensure that appropriate safeguards are in place and it provides value for money.
- Key Performance Indicators for the service should be outlined and monitored such as impact on training, expertise of hospital and community clinicians and keyworkers and health outcomes on babies.
Acknowledgments
The joint community neonatal clinic held at Colham Manor Children’s Centre was made possible by so many people. I am immensely grateful to these colleagues (and more!): Ms Samantha Blunn, Ms Laura Laryea, Ms Claire Fry, Ms Helen Davies, Ms Tahira Noordin, Mrs Faye McLoughlin, Mrs Caitriona Delaney, Ms Yvonne Arnold, Ms Josanne Hampton, Ms Chris Mann, Ms Kate Wilson, Ms Ashifa Trivedi, Mr Vishal Mehta, Mr Nigel Goss, Mr Matt Kybert Dr Devangi Thakkar, Dr Elizabeth Lek, Professor Abbas Khakoo, Dr Tristan Bate, Dr Ranjith Govindan, Ms Nikki Jackson, Ms Gubby Ayida and a special thanks to Rt Hon David Simmonds CBE MP for Northwood and Pinner.
And finally, to Manraj, Gurmehar, Gurbani, Jahvon, Roseleen, Orla and Aoife and their parents without whom this clinic would never have seen the light of day.
Dr Jide Menakaya, Consultant Paediatrician Hillingdon Hospital
A Partnership project of The London Borough of Hillingdon, The Hillingdon Hospitals NHS Foundation Trust and Central & North West London NHS Foundation Trust.
Published: February 2021
