Action
By identifying families in need, advocating for child health priorities and connecting to community resources, we can take action through small steps to encourage local engagement and empower families to thrive together.
Key learning points
We all need to play our role in tackling the social determinants of children and young people's health and creating health equalities.
For every patient we can screen, ask, listen and prescribe local resources to help.
Getting started
The social determinants of health can seem like an insurmountable problem and we can often feel small and powerless against it. We see children living in poverty in A&E, clinic, inpatient wards and intensive care units every day. We need to treat poverty as a key risk factor for disease if we want to improve a child’s quality of life and long-term health outcomes, and we can each play a key role in identifying and reducing the impacts of poverty for every child we see.
Just as screening is important for other adverse risk factors like smoking or domestic violence, we can also screen for poverty. By identifying low-income and/or vulnerable families, we can connect them to local resources and community support, which could be vital in helping increase participation, provide essentials and empower families to thrive together.
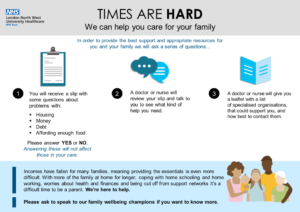
Talking about income is a delicate subject. Incorporating simple screening questions that all parents and carers are asked can help identify families who need help. Families are often relieved that we recognise the impact of poverty on their child’s health and when we want to offer them assistance.
We can use the routine family and social history we already take to identify risk factors. These include: families with three or more children, single parents/carers, unemployment and/or parents with chronic physical or mental health conditions. If you are familiar with the HEADSS psychosocial assessment tool for adolescents, first published by Cohen et al. in 1991, you can adapt this to both identify and discuss the impact of poverty with families with children of all ages.
The adapted “HEADSS” tool
Home
Who lives at home with you?
- Chronic physical or mental health problems
- >3 young children
- Single parent/carer
What is your house like?
- Housing concerns
- Pests, leaks, mould, cold, overcrowding
-
Employment/Education
Do you work? What is your job?
- Unemployment/low income
- Asylum seekers, travelling community
How is your child doing at school?
- Developmental delay
- Poor school attainment
- Poor attendance
-
-
Activities
Do you have any family hobbies?
Have you been on holiday together in the last year?
- Lack of disposable income or access to transport
- Social isolation
-
Diet
What did you eat yesterday?
- Lack of (healthy) food
- Unable to afford fresh fruit and vegetables
- Parents missing meals to feed children
In the last year, have you worried that your food would run out before you got money to buy more?
- Free school meals
- Foodbank use
-
Safeguarding/support
Have you ever had a social worker?
- Reasons for social worker could give insight into current and previous vulnerabilities.
- Consider what support they already have?
- Are they receiving benefits?
Has anyone ever hurt or threatened you and your family?
- Physical, emotional, sexual abuse or neglect warrants further investigation and referral as per local pathways
How can I help a child and their family?
Sometimes just being understanding of the family’s social and financial situation and empathetically managing their child’s healthcare in that context can be enough to transform the quality of a child’s care.
There are other specific actions you and your teams can also take:
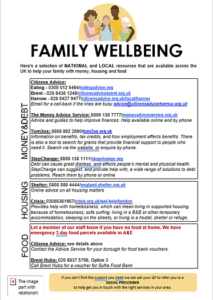
Signposting parents/carers to services that focus on the social determinants of health is an increasingly important skill for all health professionals. This may involve directing them to sources of financial support, both from the state (such as statutory benefits and social security entitlements) and third sector organisations (local food banks, childcare support, and other practical services). Your local council website is a good place to start to identify any resources available locally and/or explore what is available via local “early help” services and consider a referral.
Empower families and encourage their strengths on an individual level (personal resilience, knowledge and skills) or community level (family and social networks, schools and clubs, and third sector organisations).
Adapt and adopt template posters and leaflets to sign-post to local organisations and resources offering help and support. Some examples are listed below with templates available to download and edit to your own local requirements:

Introducing screening and signposting projects into your clinical department
For the children who come through our A&E and clinic doors and the neonates that we see in our NICU or on whom we conduct NIPEs, inequality is a hidden co-morbidity. On top of our daily clinical workload as paediatricians, this additional pressure to tackle yet another concern for our patients seems overwhelming.
We may be able to recognise the signs of struggle when we are taking a history, see the family dynamics during an inpatient stay or even have a direct account from the patient or their family about the condition of their housing. There are many ways in which we can help them, and it starts with us acknowledging that we have a part to play.
Identify key stakeholders for a quality improvement project
Although you may need to develop your quality improvement project plan before you address key stakeholders in person, it is important to think about who you will need as partners early on if you want your project to be successful and sustainable.
Depending on your hospital / department this may vary, but may include:
- Colleagues keen to help with introducing screening and sign posting
- Medical staff – clinical director, department consultants, SHOs and registrars, nursing staff (matron, senior team, nurse educators)
- Safeguarding team may have ideas on how to link screening into existing ways of supporting families e.g. “cause for concern e-form” linking with wider hospital patient advice and liaison teams or social services “early help teams”
- Existing support services for families e.g. Bristol Royal Hospital for Children LIAISE team offer practical support on accessing income and essentials to families with children who have been admitted to hospital for prolonged periods of time
- Local council partnerships – there may be funding available in your region to support projects that try to increase integrated care, linking medical services with social services and charity partners. Search for key contacts working for families and young people in your local Sustainability and Transformation Partnership and/or Integrated Care System
- Local GP services may have social prescribing services for adults, with some Clinical Commissioning Groups offering social prescribing resources for young people too
- Local universities may have departments with relevant expertise as well as experience in research and knowledge of funding opportunities e.g. University of Bristol, Bristol Poverty Institute has been a useful point of contact for linking with local organisations and partners within the council as well as considering opportunities for funding in the future
It is important to email the organisations you are planning to include on your resources leaflet to check that they are happy to receive referrals but can also be an important way to learn more about what resources are available for families.
Design your screening questions
Introduce a HEADSS tool or adapt questions into your own local proforma. For example, key social needs screening questions have been identified by an evidence-based tool created by Health Leads in the US, including:
- In the last 12 months, did you ever eat less than you felt you should because there wasn’t enough money for food?
- In the last 12 months, has the electric, gas, or water company threatened to disconnect the supply in your home? Or have you been worried that you wouldn’t be able to pay your bills?
- Is your housing unstable or are you worried that in the next 2 months, you may not have stable housing?
- Do you have any urgent needs, for example you don’t have food and/or a place of shelter today? Would you like to receive assistance with any of these needs?
Design your resources
Adapt and adopt example leaflets and/or posters. You may want to use a booklet format or a one page poster format. As well as leaflets, you may want to have resources available as posters viewable in the emergency department or hospital wards.
Looking on your local council website can help identify what resources are available locally. We would recommend taking a bit of time to familiarise yourself with the organisations and what they have to offer.
Patient participation and feedback from families is really important. If you have access to patient participation groups it is great to get their input. Or you could get feedback from families and improve and refine your resources as you progress through Plan-Do-Study-Act cycles as part of a local quality improvement project.
Remember: Depending on where you work you may need to get any new documentation checked with the information governance team.
Here are some useful programmes of support we can tell families about:
Turn2us is a national charity providing practical help to people who are struggling financially. Their ‘Benefits Calculator’ takes less than 10 minutes to complete and it will tell families which means-tested benefits they may be entitled to, including tax credits. The ‘Grants Search’ can also help families look for funds that may be able to provide a grant or other types of help, and they also award their own grants from the Turn2us Elizabeth Finn Fund, the Turn2us Response Fund, and the Turn2us Edinburgh Trust.
Support is also available through their helpline: 0808 802 2000 (09.00 am – 17.00 pm Mondays-Fridays).
Supporting the #EndChildFoodPoverty campaign, Full Time Meals by Marcus Rashford and Tom Kerridge, provides weekly simple and inexpensive recipes to equip families with the skills to get the most out of the Healthy Start vouchers.
Community Fridges aim to bring together those with surplus food (from businesses and individuals) with those in need of access to food. It is hosted by ‘Hubbub’ who currently co-ordinate the use of 250 community fridges around the country. This social enterprise is not only great for families struggling with the increasing cost of living, but also a way to reduce waste.
It began in 2016 in Derbyshire and in 2022, they partnered with the Co-op to continue supporting local communities. This project also offers cooked meals as well as workshops on cooking, growing plants and clothes swaps. This is a great vehicle to help communities support one another and build local networks.
Home Start is a volunteer-led organisation which supports families by attending their homes and helping them navigate parental duties. They also provide programmes aimed at boosting development in children from a very early stage.
The Home Start volunteers are also able to support families to access local services in their area (housing, citizen advice, financial advice, etc). Home Start is a charity operating across the UK and they have an easy locator on their website.
This organisation provides families with white goods such as fridge/freezers, washing machines and cookers. Families struggling to provide a safe and clean environment for their children will be able to make use of the services provided by this charity and can be referred through the local food bank or alongside social services.
This is an online course offered by the UK based charity OnePlusOne (with Dame Judy Dench as patron). It aims to help first-time parents with the difficulties they may face as they adjust to their new lives as parents and reduce domestic violence in those sleepless and trying times.
They also offer a number of other courses which are aimed at reducing parental conflict. This is a very helpful tool to recommend to families in the NICU setting with other courses also offered by the charity to be considered for parents of older children.
These are usually set up and run by local councils, but in certain areas there are business which also run sessions to support breastfeeding mothers. They are a great way for mums with new-borns to connect with others in a similar position and share valuable advice among each other. They are a free resource and it often involves cake being consumed!
Check your local authority website and social media platforms to find breastfeeding cafes in your region.
Tell people about your project
Introduce and evaluate your project with stakeholders to continually adapt and improve your interventions to ensure they become embedded in to the culture of your local department and clinical team. For an example on how to successfully implement a quality improvement project on the social determinants of children and young people’s health, read ‘Poverty in Practice’ by Singh et al in the Archives of Disease in Childhood.
You can also use template teaching resources for grand round / journal club to share your work. Here are some examples below for you to download and adapt for use in your own clinical environments:
This page was created by Dr Hannah Zhu, Dr Emma Sunderland, Dr Akudo Okereafor, Dr Irnthu Premadeva, Dr Guddi Singh and Dr Helen Leveret from the Wellbeing and Health Action Movement community.
References
Cohen E, Mackenzie RG, Yates GL. HEADSS, a psychosocial risk assessment instrument: implications for designing effective intervention programs for runaway youth. J Adolesc Health. 1991 Nov;12(7):539-44. doi: 10.1016/0197-0070(91)90084-y. PMID: 1772892.
