Children’s Outpatients Reopening Post-COVID19
A rapid quality improvement project to restart outpatient services at Great North Children's Hospital following the impact of COVID-19.
The Problem
On March 23rd, 2020 the UK government announced a national lockdown to limit the spread of COVID-19. This meant all elective hospital activity was postponed. This is a brief outline of the challenges faced in restarting the Great North Children’s Hospital (GNCH) outpatient department (OPD) and Child Development Centre (CDC) to protect staff and patients, and to accommodate government mandated social distancing to prevent the spread of COVID-19.
Major stakeholders involved in the project were:
- Patients and their families.
- Multi-disciplinary teams with their different needs who use the shared space.
- Outpatient staff and management team.
Aim
Re-engineer children’s outpatient services for the COVID-19 era so patients feel safe, are safe and get the care they need.
- Outcome measures – patient feedback, and the waiting time from referral to consultation (face-to-face or remote) and to treatment.
- Process measures – activity level and staff feedback.
- Balancing measures – the ‘Was Not Bought’ rate, and separate pieces of work being done by colleagues at GNCH looking at various side effects of lockdown on children e.g. Changing patterns of safeguarding referrals. Are children presenting to our ED later and more ill than before?
Making the Case For Change
Previous levels of outpatient activity by specialty were determined using pre-COVID clinic lists, and a similar total number of paediatric outpatient clinic slots were reallocated to each specialty (Figure 1). Five clinic sub-areas (A, B, C, D and CDC) were previously mixed specialties with a lot of crowding. In the new structure, each specialty amalgamated their weekly clinics in whole sub-areas and was asked to re-organise and maximise clinic slots using a blend of remote (phone/video) and face-to-face consultations. This also required major re-organising of multi-professional healthcare staff to alter their pre-existing schedules against a new template.

Figure 1: Previous and proposed clinic allocation percentages by specialty.
Slots were staggered with sufficient gaps to prevent overcrowding in each sub-area. We estimated approximately 180 patients maximum could be seen per day (18 patients in AM and 15 per PM slot, per area) alongside the procedure clinic. Compared to pre-COVID, this was a 55% reduction in face-to-face outpatient capacity.
A lot of work was spent collecting data. A request was submitted to our information services team and we used some automatically collected data from our appointment system. With near real-time data, activity levels can rapidly be used to make fine adjustments to level quieter and busier times (Figure 2).
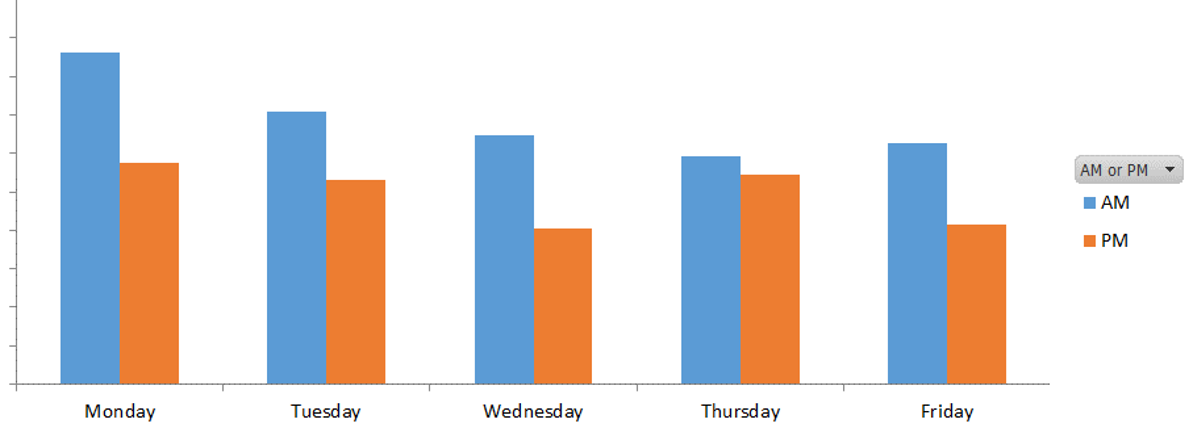
Figure 2: Number of face-to-face clinic attendance by time and day in one week.
Our Improvement
The ‘Was Not Brought’ rate remained low after reopening indicating we were likely to be selecting the right patients to attend face-to-face consultations, and teams were contacting families that wished to have remote consultations instead (Figure 3). For some children, being seen face-to-face was important for safeguarding purposes.
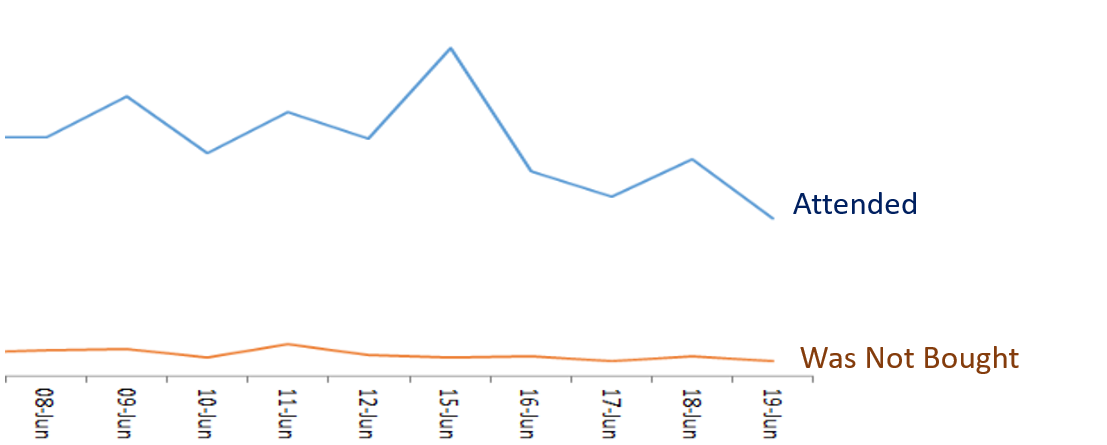
Figure 3: The number of attended and ‘was not brought’ patients at clinic per day.
To ensure patients felt safe and comfortable attending face-to-face appointments at GNCH, all attending patients were invited to complete a short anonymous survey. These were handed out at reception and a QR code was added linking to an online survey to enable touch-free responses online via smartphone.
Responses were collated weekly and distributed to outpatient and management staff to rapidly inform improvements (Figure 4). As of June 25th, 2020 we received 169 responses from patients and parents over three weeks of data collection. Feedback was positive and patients felt safe from infection whilst attending face-to-face outpatient appointments.

Figure 4: Patient feedback newsletter published for week commencing 15th June 2020.
Staff feedback was also collated weekly and directly informed efforts to improve clinic processes, scheduling and layout (Figure 5). Computer and IT delays were identified that impacted on patient flow, and this was escalated as a priority with new computers now being installed. Positive feedback was a great motivator to outpatient staff who owned the data and owned the change.

Figure 5: Staff feedback newsletter published for week commencing 15th June 2020.
Learning and Next Steps
- Outpatients never closed during COVID-19. Staff worked very hard to maintain essential urgent face-to-face consultations and this needs to be acknowledged. Reopening just meant increasing activity in a planned way to maximise capacity.
- Infrastructure to support remote consultations (especially regional nurse procedure clinics and home medication delivery) need to be in place and useable to create capacity for face-to-face consultation.
- The change period was unsettling. Twice weekly, then weekly GNCH COVID updates/consultations were a great enabler for a smooth restart.
- Listen to feedback from patients and staff as they see the barriers, and the solutions.
- Live data collection enabled rapid improvements and real-time feedback
Thank you to all the clinical teams at Great North Children’s Hospital for their patience and support. Special thanks to all staff in children’s outpatients and the Child Development Centre – Jo Fell and Becky George who made this all possible, Chris Vickers for facilitating the QI aspect and James Holt for QI data collection and analysis.
Project Lead: Dr Yincent Tse, Consultant Paediatric Nephrologist
Organisation: The Great North Children’s Hospital – The Newcastle upon Tyne Hospitals NHS Foundation Trust
Published: August 2020
