Optimal Cord Management in preterm infants – a Quality Improvement project
A low-cost project that a multidisciplinary team at Singleton Hospital implemented to improve rates of optimal cord management in preterm babies. This work highlights how data from the National Neonatal Audit Programme was used to improve quality of care.
Davies G, Senior ANNP, Cosgrove E, ST2, Makri V, Consultant Neonatologist, Webb J, Consultant Neonatologist; Singleton Hospital, Swansea Bay Health Board
Background
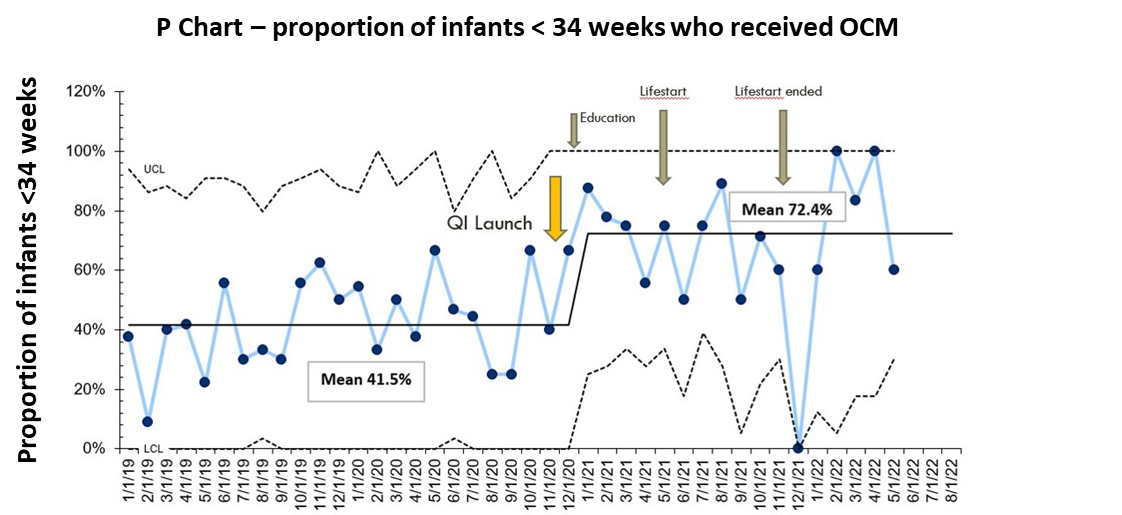
Evidence shows that Optimal Cord Management (OCM) leads to improved outcomes, including reduction in mortality in preterm infants. In 2020 Singleton Hospital NNAP results showed that OCM was achieved in only 34.5% of preterm babies born at less than 32 weeks’ gestation. Retrospective analysis of 24 months of Badgernet data, focussing on preterm infants of less than 34 weeks’ gestation, confirmed low rates of OCM locally.
Therefore, a team was put together to facilitate a Quality Improvement project (QIP). Our SMART (specific, measurable, achievable, realistic, timely) aim was to raise the baseline rate by 40% over the first year, following which we would establish a new baseline and agree a new SMART aim. Challenges to providing OCM are well recognised, particularly for preterm babies.
Measures
OCM was defined as waiting at least 60 seconds before clamping the umbilical cord. A QIP was undertaken collaboratively with members of the Neonatal, Obstetric and Midwifery teams and OCM audit forms were launched with the aim of analysing possible barriers and improving practice.
These forms prompted the delivery team to document the infant’s gestation, mode of delivery, condition at birth and temperature on the Labour Ward and on admission to the Neonatal Unit.
Our improvement plan
Interventions were focused on improving awareness and understanding of the benefits of OCM in preterm babies amongst the delivery team. QI methodology using ‘plan, do, study, act’ (PDSA) cycles was used and applied to each intervention.
These interventions included:
- displaying posters on the Neonatal Unit and Labour Ward
- providing targeted teaching sessions
- parental discussions within antenatal counselling, and
- introducing OCM planning to the pre-caesarean section of the World Health Organisation (WHO) checklist.
Our first PDSA cycle targeted at increasing awareness amongst the professionals, had a very positive impact in raising our OCM rates. However, we soon realised the importance of providing continuing education to ensure that all new staff members within the Multidisciplinary Team (MDT) were made aware of our QIP. The variation in practice that was initially noted, improved significantly after introducing our next PDSA cycle, namely including the plan for OCM to the pre-caesarean WHO checklist.
Our final PDSA cycle was the introduction of the Lifestart trolley with the aim to further improve OCM among the more challenging group of compromised preterm infants requiring respiratory support. The Lifestart trolley was available for 5 months, but it was used very infrequently due to logistical difficulties. Since our OCM rates increased irrespective of its use, we agreed to investigate different and hopefully simpler systems, which can help facilitate lung inflation and optimize respiratory management in infants who do not breathe spontaneously following birth.
Outcomes
Data on compliance with OCM since the implementation of our interventions were collected over 8 months. Results to date show an increase in monthly mean compliance with OCM from 41% pre-intervention to 72% post-intervention. Normothermia rates remained the same pre- and post-intervention.
Challenges and learnings
Working with multiple different professionals posed difficulties, as it was essential to achieve agreement before implementing a change in practice. This was overcome by frequent multi-disciplinary staff meetings, which addressed any differences in opinion and ensured smooth collaborative working. A further challenge we faced was acknowledging staff rotations and ensuring education of all new staff members.
However, the fact that permanent team members were the driving force of this QIP, improved continuity and increased the sustainability of the positive effect of this intervention.
Top tips for implementation
This was a low-cost QI project that can easily be implemented across other units providing they have passionate multidisciplinary team members willing to adopt OCM.
Acknowledgements
This project would not have been possible without the support of all members of Singleton Hospital Neonatal, Obstetric and Midwifery teams.
